
Finally found a PPE regimen that seems to work well. This is the Envo mask (envomask.com) and the Wiley-x SG-1 goggles (sporteyes.com/wiley-x-ssg-1.…). A few notes (thread): #medtwitter #FOAMcc #COVID19 
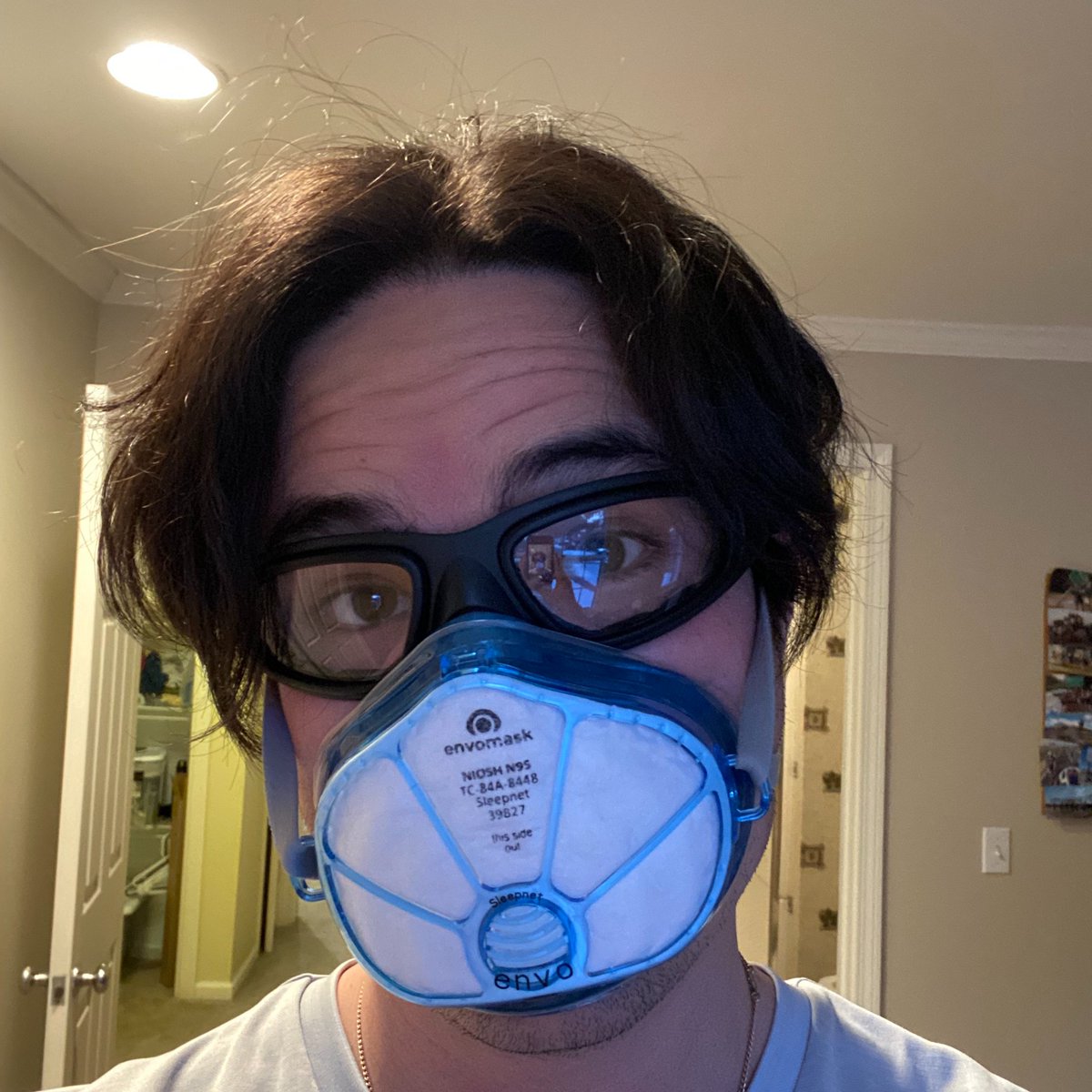
1. The goggles are not 100% sealed and have small vents along the sides. However, I do not think a 100% seal is necessary, and would be an incredible fog-creator. The Wileys are also pricey; consider these, almost as good (amazon.com/gp/product/B00…) but don't seal quite as well.
2. Any goggles, regardless of coating, will fog. Most important is a good mask seal, then use an anti-fog treatment. I found sprays to be a bother, but wipes are good. Try: sporteyes.com/hilco-fog-bust…
3. The Envo mask is comfy (although the gel seal feel sticky after a while), N95 certified, and the exp. valve comes with a plug to seal it. However, it is not "on label" for healthcare (it's for occupational health) and has now been banned by our hospital for that reason. Bah.
4. Try not to clean ANY goggles with any wipes except pure alcohol and ideally, probably not even that. The plastic will eventually degrade and develop that hazy fog. I've been using a UV box for cleaning and that seems to work well.
• • •
Missing some Tweet in this thread? You can try to
force a refresh


