Case report of a hospital COVID-19 outbreak probably caused by airborne transmission. A child with an infected mother was admitted, after which 6 healthcare workers, 2 child patients, and 1 parent tested positive.
H/T: @CPita3 via @lisa_iannattone.
academic.oup.com/ofid/advance-a…

H/T: @CPita3 via @lisa_iannattone.
academic.oup.com/ofid/advance-a…
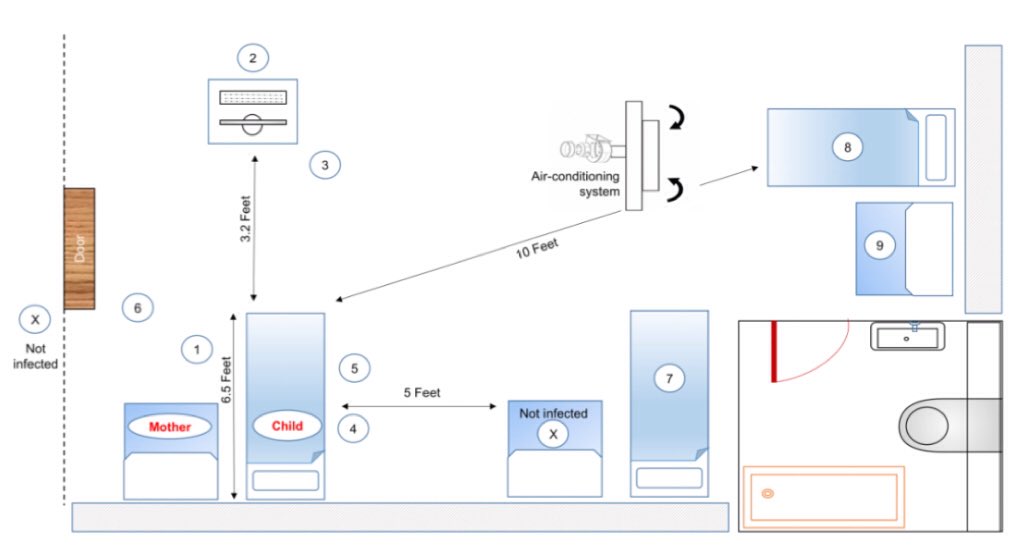
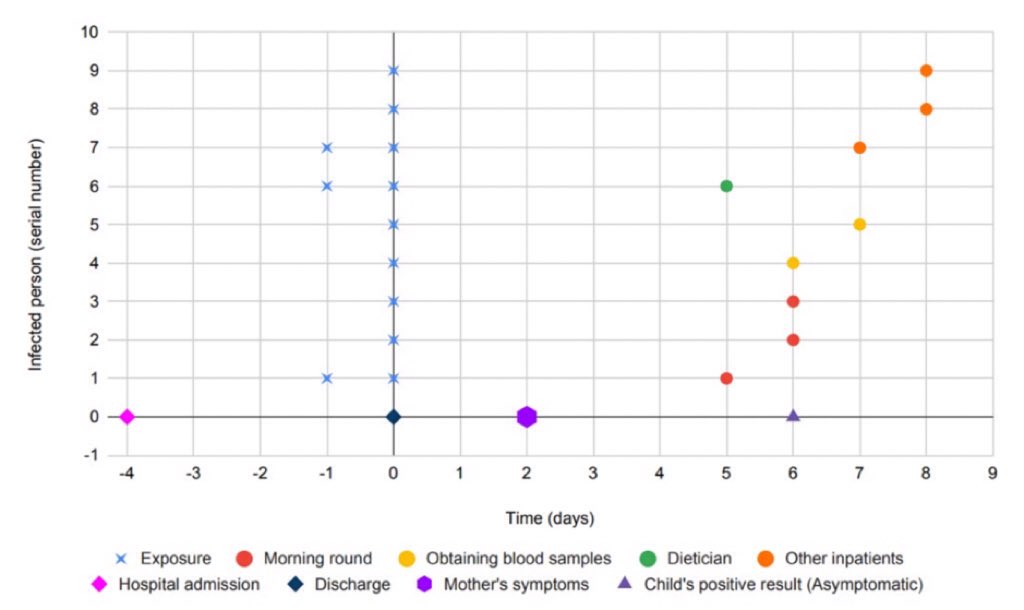
Three of the 6 healthcare workers had no direct contact with the mother or child and maintained a distance of approximately 2 metres during a ward round and dietician consultation. All 6 wore surgical masks. No aerosol-generating procedures were performed.
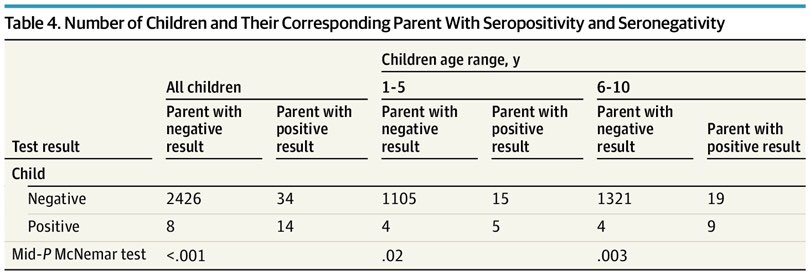
An additional 3 out of 4 contacts (2 child patients and one mother staying in the same room) tested positive. They were staying at a distance of more than 2 metres from one another, although brief contact over a shorter distance cannot be ruled out.
During the morning ward round, the child was asymptomatic and did not cough, sneeze, cry, or talk. The child tested positive 10 days after admission (6 days after most people were exposed), but remained asymptomatic.
The mother tested positive 8 days after admission (2 days after she developed symptoms). The authors believed the mother to be the index case, and that she transmitted the virus by talking. However, it's not possible to rule out the child.
Interestingly, the authors thought the child's young age (3 years), lack of symptoms, negative test on admission (4 days before most people were exposed), and subsequent positive test after the mother, made him unlikely to be the outbreak source.
In fact, none of these factors rule out the child, and it's disappointing to see some misconceptions about children repeated here.
The child's case probably would have gone undetected if the mother (and other adults) had not shown symptoms, which prompted the child's testing.
The child's case probably would have gone undetected if the mother (and other adults) had not shown symptoms, which prompted the child's testing.
Although the mother is the most likely source (because the timing of her symptoms would have likely made her highly infectious at the time most people were exposed), it's possible that both the mother and the child could have transmitted the virus.
The most important finding of this case report, is that physical distancing and the use of surgical masks were inadequate to prevent this particular outbreak. While surgical masks do offer protection, they do not provide the same level of protection as a P2/N95 mask.
Additionally, at least two of the secondary cases (a doctor and nurse) had only 10 minutes exposure (when they collected blood samples from the child).
In summary, this case report demonstrates that airborne transmission of SARS-CoV-2 occurs, and that less than 15 minutes exposure is sufficient to become infected.
• • •
Missing some Tweet in this thread? You can try to
force a refresh