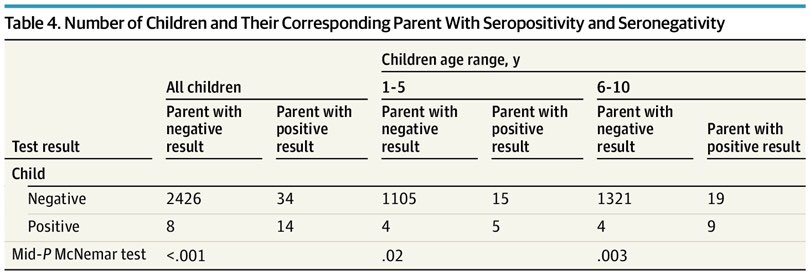
(1/17) Study of 2482 parents and 2482 children aged 1-10 years from Baden-Württemberg, Germany, showing that between 22 April and 15 May 2020, parents were more likely to have antibodies against SARS-CoV-2 than children (1.9% vs. 0.9%).
jamanetwork.com/journals/jamap…
jamanetwork.com/journals/jamap…
(2/17) In 56 families where at least one parent or child had antibodies, the combination of a positive parent and negative child was 4.3 times more likely than a positive child and negative parent. 
(3/17) On the surface, this might sound like children are less susceptible to infection, and are less likely to transmit the virus than adults.
This is a genuine possibility, but I think there’s another, better explanation.
These weren’t just any parents...
This is a genuine possibility, but I think there’s another, better explanation.
These weren’t just any parents...
(4/17) This was a convenience sample (participants were self-selected), and 22% of the parents were healthcare workers.
This is not representative of the general population.
This is not representative of the general population.
(5/17) In this context, it’s unsurprising that parents were more likely to test positive than children.
The parents had a high-risk occupation.
The parents had a high-risk occupation.
(6/17) The children were generally at home (because schools were largely closed), and did not have the opportunity to catch the virus, except from their parents.
(7/17) It’s also unclear if parents took any action to shield their children from infection.
With so many being healthcare workers, and knowing they might bring the virus home, it’s possible they altered their behaviour to protect their children.
With so many being healthcare workers, and knowing they might bring the virus home, it’s possible they altered their behaviour to protect their children.
(8/17) We also know that most people infected with SARS-CoV-2 don’t transmit it to anyone.
This includes the household setting. People often don’t infect their family members.
This includes the household setting. People often don’t infect their family members.
https://twitter.com/drzoehyde/status/1306635443262218240?s=21
(9/17) So, we should not be surprised to find an imbalance between infected parents (one-fifth of whom were at high risk of infection owing to their job), and less infected children (who had limited opportunity to become infected because they didn’t go to school).
(10/17) An additional issue to consider, is whether all infections were detected.
The authors had a high number of borderline results they classified as false positives.
The authors had a high number of borderline results they classified as false positives.
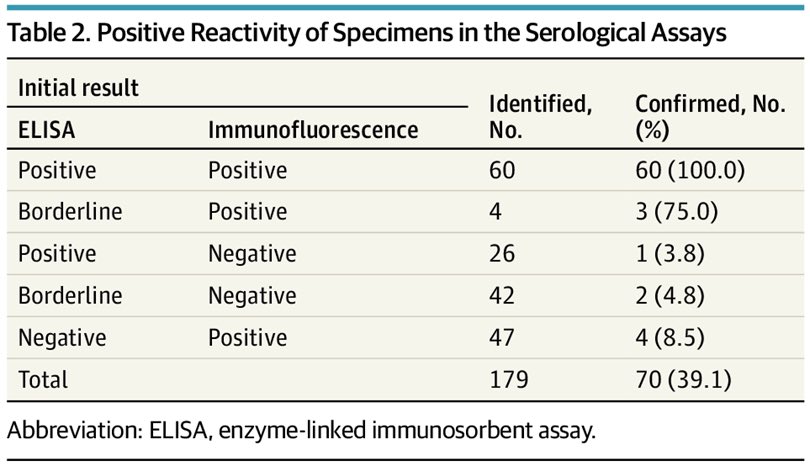
(11/17) This may have been correct, but it would have been interesting to see if children were more likely than adults to have a borderline result, and to have their results reclassified in this way (from positive to negative).
(12/17) Children have a less broad antibody response than adults, and false negatives are more likely in children.
https://twitter.com/drzoehyde/status/1324386054443429888?s=21
(13/17) The authors say their findings indicate “children are very unlikely to have boosted the COVID-19 outbreak in southwest Germany during the period of investigation.”
But it must be noted this was during a period of school closures.
But it must be noted this was during a period of school closures.
(14/17) The authors go on to compare this to influenza, noting children frequently transmit that virus.
But this is not a fair comparison, because SARS-CoV-2 was not circulating widely in children at the time of the study, and they had limited opportunity to become infected.
But this is not a fair comparison, because SARS-CoV-2 was not circulating widely in children at the time of the study, and they had limited opportunity to become infected.
(15/17) In summary, I don’t think the study tells us anything about the biological susceptibility of children to infection, and the authors themselves conclude that nothing can be said about the infectivity of children.
(16/17) What the study does tell us, is that parents (especially healthcare workers) who go to work are more likely to get infected than children who largely stay home (or only go to childcare at a time when the virus is not widespread in children).
(17/17) We can’t use this study to say that children are less susceptible to infection, or that schools are “safe.”
The safety of schools depends on the level of community transmission, and whether precautions have been taken in that setting (masks, ventilation, etc.)
The safety of schools depends on the level of community transmission, and whether precautions have been taken in that setting (masks, ventilation, etc.)
This may be of interest to you, @KMonkemuller. I think you were asking about this study the other day. I’ve only just had time to read it.
• • •
Missing some Tweet in this thread? You can try to
force a refresh