1. Today is #WorldCancerDay our analysis led by @dr_mosama & @hvanspall academic.oup.com/ehjacc/advance… with @AnaBaracCardio @islamelgendy83 @DLBHATTMD @adnanalkhouli @safinmc @dataevan studies disparities in care & outcomes of cancer pts presenting with STEMI @DrMarthaGulati @ShrillaB 
2. #WorldCancerDay It builds on our work published last year led by @adityadoc1 showing pts with cancer less likely to be managed invasively, and when they are have better outcomes. academic.oup.com/eurheartj/arti… @MKIttlesonMD @ovidiogarciav @DrPeterOKane @SukhNijjer @CardioIAN 



3. #WorldCancerDay The greatest incidence of AMI in cancer pts is within 30d of Ca diagnosis, many treatments can ⬆️risk aswell as shared risk factors. We sought to study whether STEMI pts with cancer are less likley to get PPCI & whether they benefit academic.oup.com/ehjacc/advance… 

4. #WorldCancerDay We used a propensity score matching approach to calculate the average treatment effect of PPCI in 5 cancers types (haematological, breast, colon, prostate and lung) and compare it to pts without cancer. Cancer pts upto 50% less likely to get PPCI @mirvatalasnag 

5. #WorldCancerDay We show that STEMI pts with cancer gain as much benefit from PPCI as pts without cancer @GlzMarcelo @DrFerNunez @MihaiTrofenciuc @GiuseppeGalati_ @VictorDayan1 @pomyers @kamleshkhunti @kamalcardiodoc1 @KTamirisaMD @_AymenAhmed @JGrapsa @IamSpurs @CardioIAN 



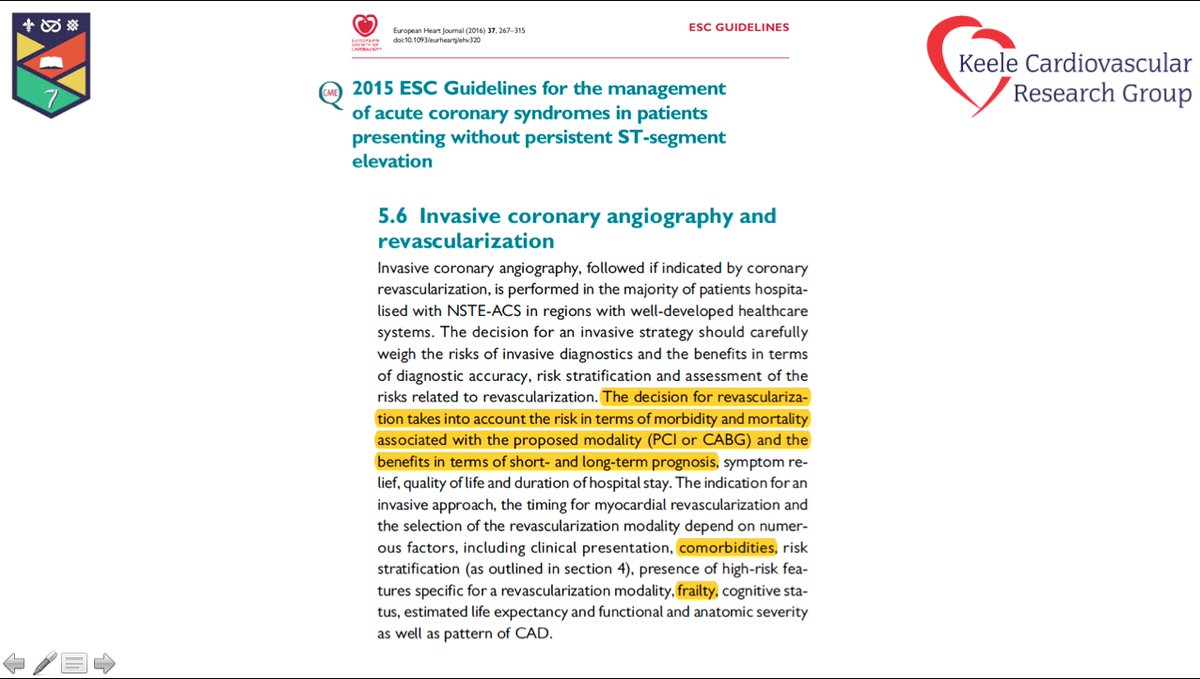
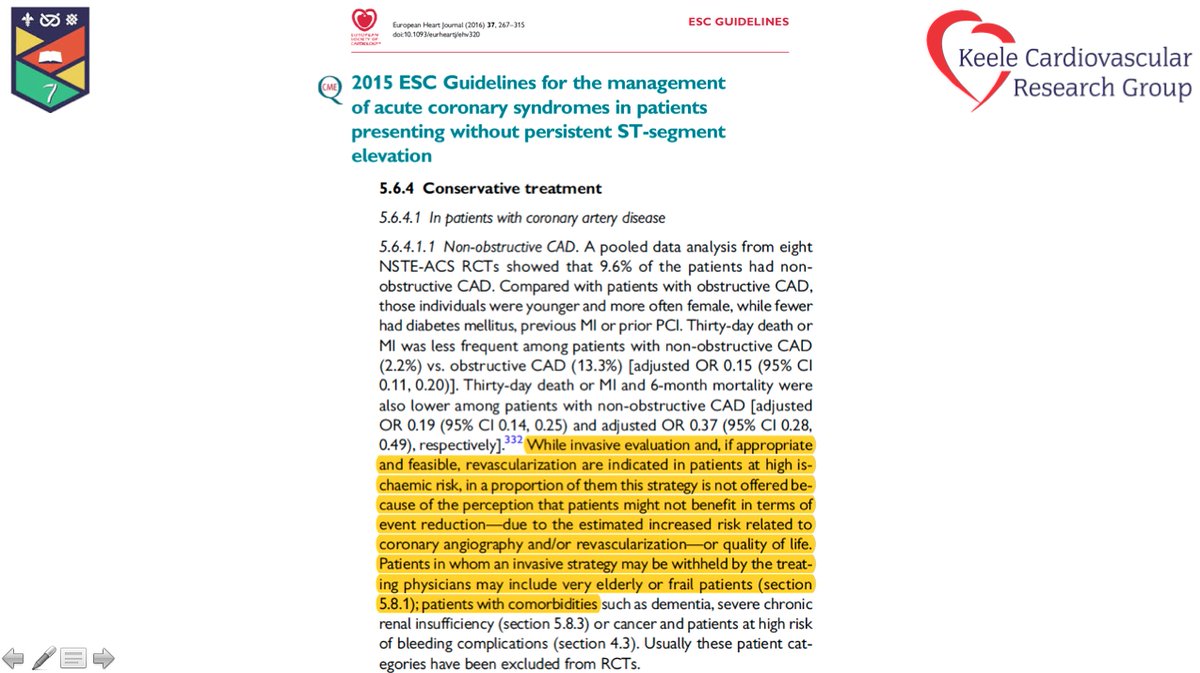
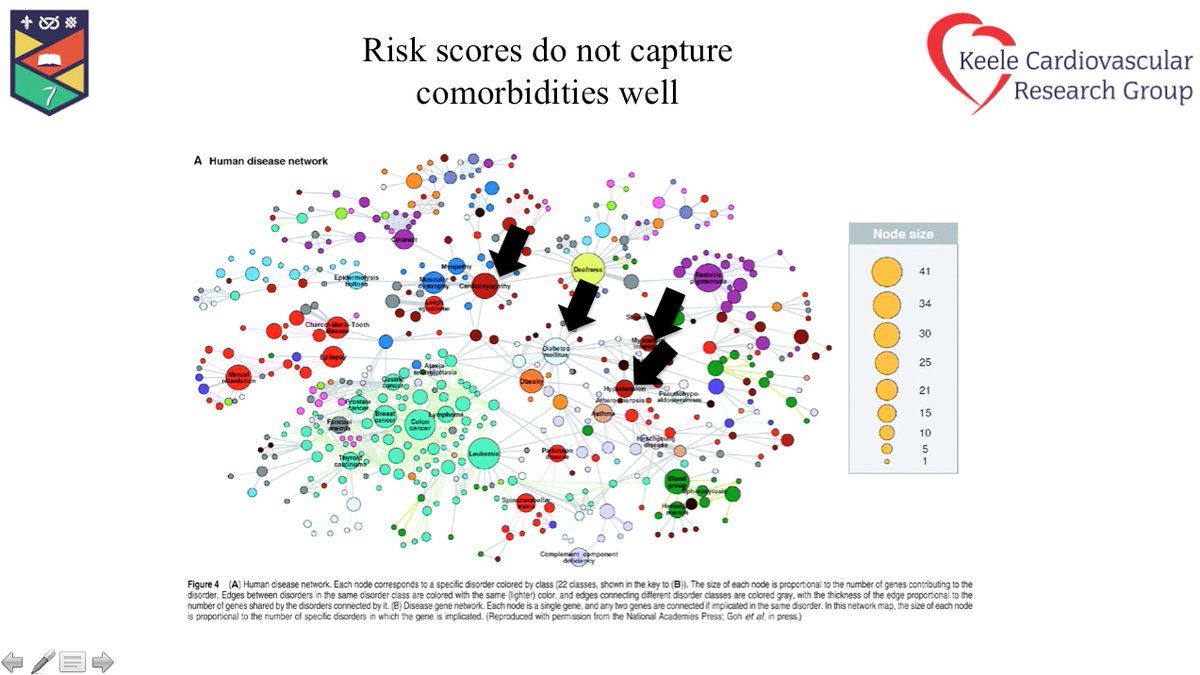
6. #WorldCancerDay Why are pts with cancer less likely to get PPCI?
🥕⬆️bleeding risk: ⬇️Clotting , low platelets, bone marrow suppression
🥕 more co-morbid
🥕 Physician bias re expected benefit, with cancer pts excluded from RCTs
🥕 ⬆️ risk of thrombotic events
@mirvatalasnag
🥕⬆️bleeding risk: ⬇️Clotting , low platelets, bone marrow suppression
🥕 more co-morbid
🥕 Physician bias re expected benefit, with cancer pts excluded from RCTs
🥕 ⬆️ risk of thrombotic events
@mirvatalasnag

7. #WorldCancerDay what can we do to optimise outcomes during / post PPCI?
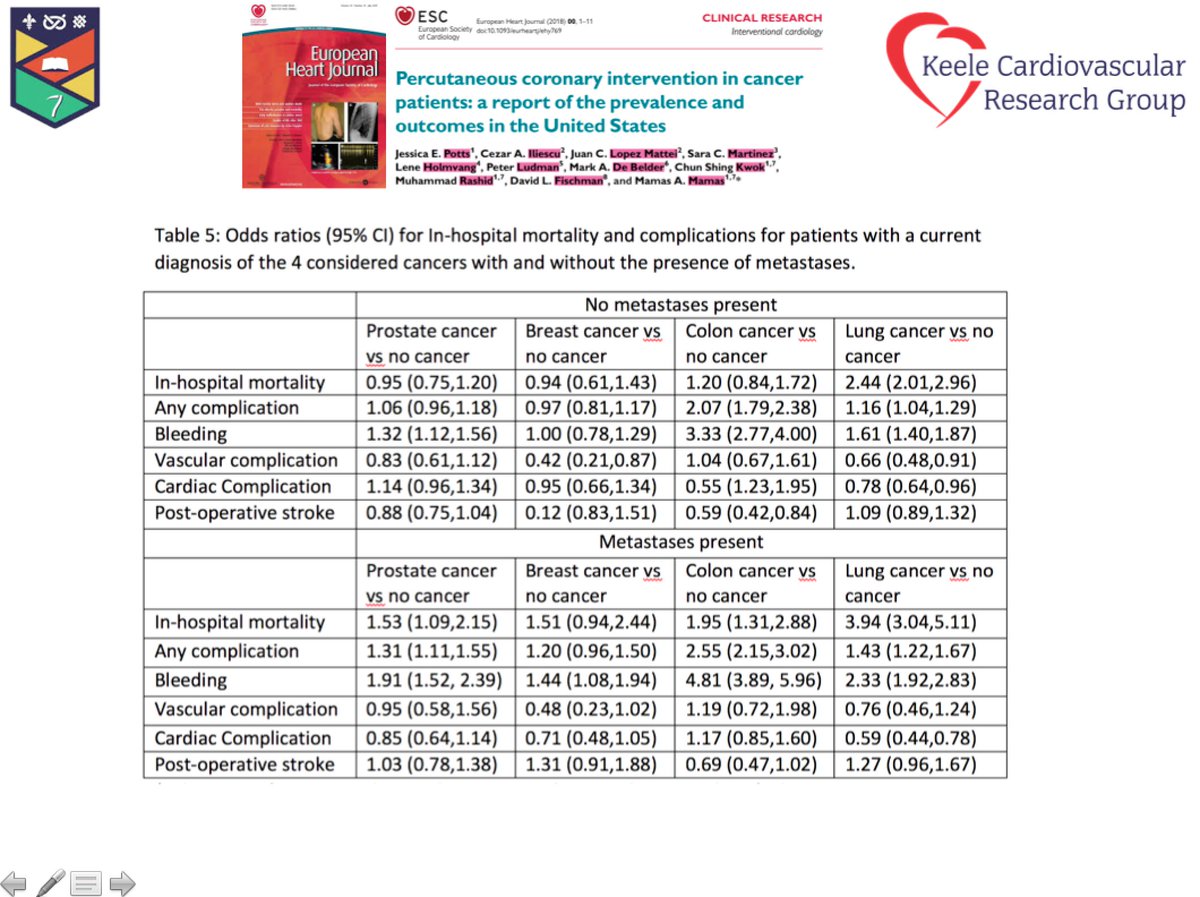
🥕 Consider / bleeding vs ischemic risk. Colon Ca⬆️bleeding, Lung CA ⬆️ischemic
🥕 #radialfirst
🥕 OCT/Image #imagefirst
🥕 use stent platforms that only require short dapt
🥕 short dapt with longer p2y12
🥕 Consider / bleeding vs ischemic risk. Colon Ca⬆️bleeding, Lung CA ⬆️ischemic
🥕 #radialfirst
🥕 OCT/Image #imagefirst
🥕 use stent platforms that only require short dapt
🥕 short dapt with longer p2y12

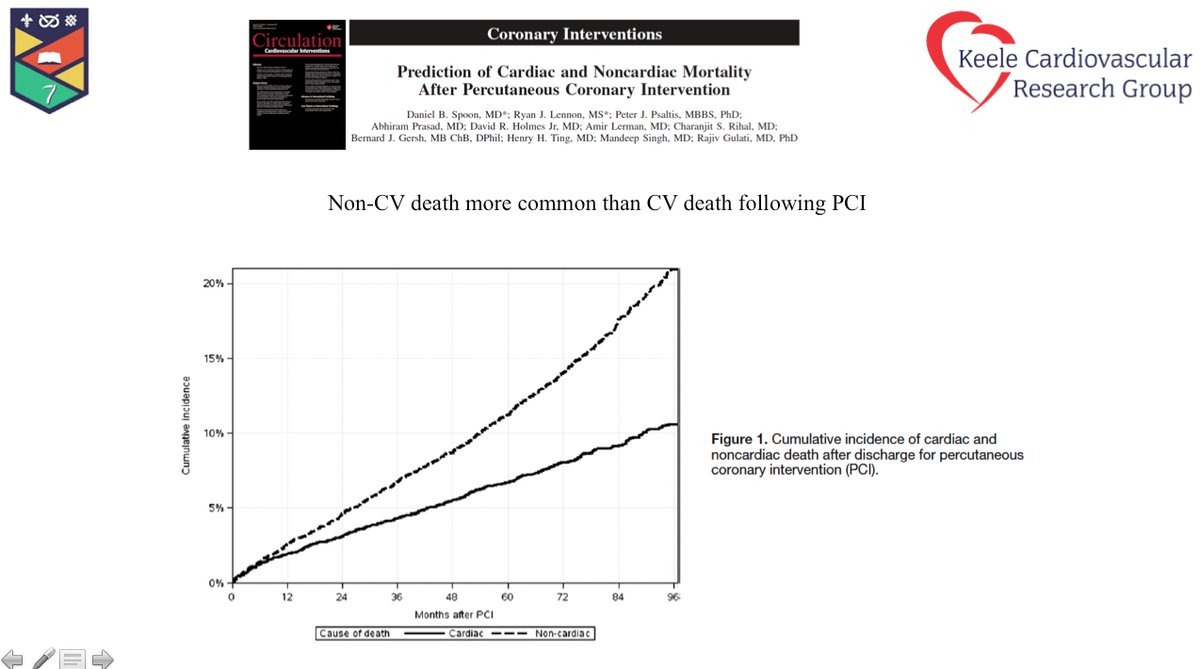
8. #WorldCancerDay In summary- Pts with cancer have as much benefit from PPCI in STEMI but are 50% less likley to receive it. CVD disease is number 1 cause of death (other than cancer) in cancer pts @AnaBaracCardio @onco_cardiology #cardioncology #CardioOncology @VivekAgarwal 

• • •
Missing some Tweet in this thread? You can try to
force a refresh