Senior Coroner for Worcestershire David Reid found that Rachel Johnston died as a result of complications of necessary surgery, to which neglect contributed
Full info here georgejulian.co.uk/2021/02/11/rac…
TLDR Lowlights (I can't bring myself to call them highlights) below
1/21
Full info here georgejulian.co.uk/2021/02/11/rac…
TLDR Lowlights (I can't bring myself to call them highlights) below
1/21
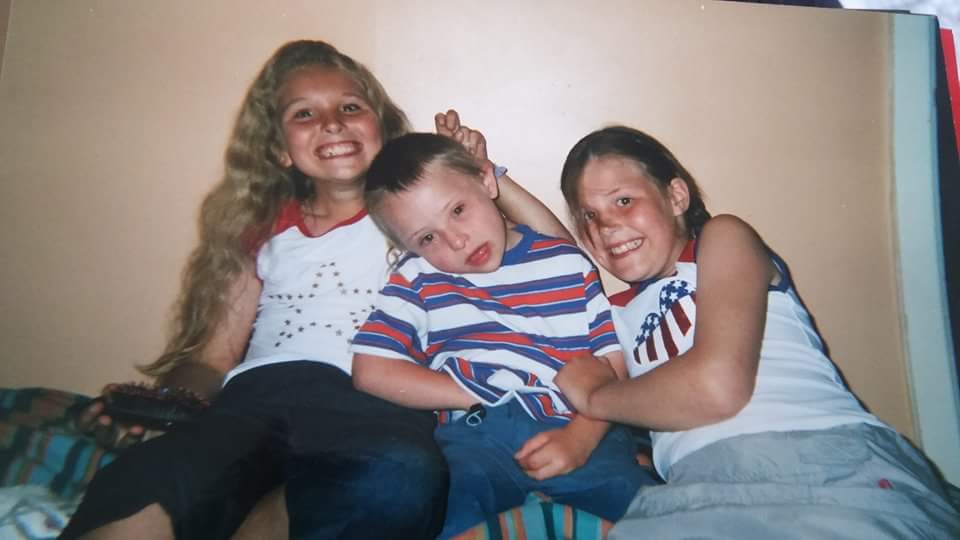
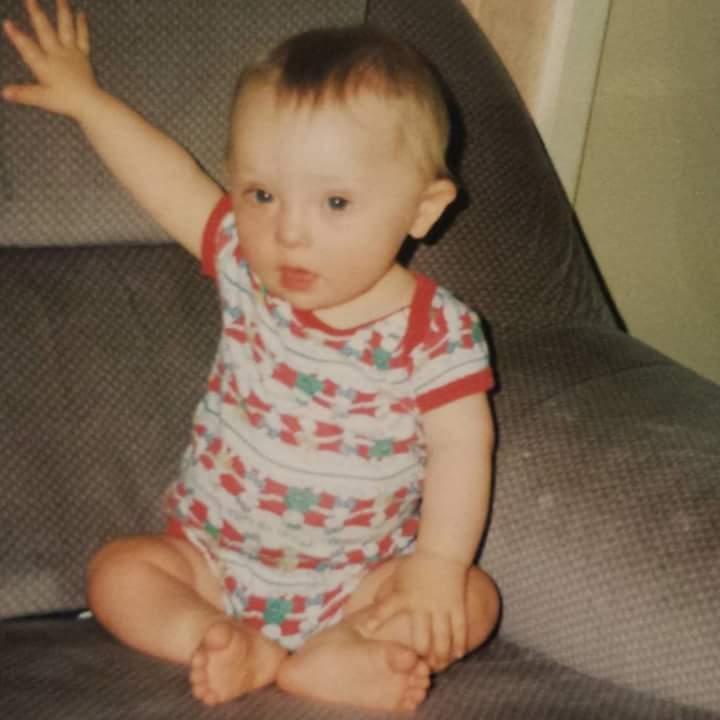
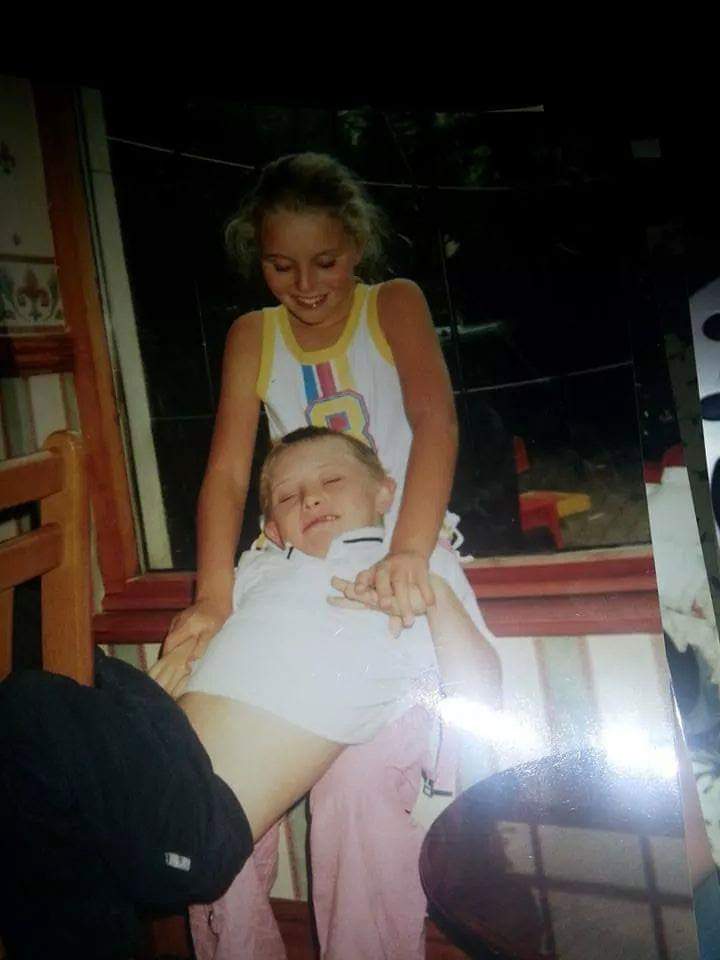
Coroner described Rachel as 'a lively and happy woman who loved music, theatre and the company of other people. She was blessed with a close family who would visit her regularly and bring her back home when there were family gatherings'
2/
2/
The Coroner accepted that Rachel’s extensive dental surgery was necessary.
He ruled on a factual dispute, and found that on discharge Staff Nurse Kate Griffiths failed to provide a leaflet about dental surgery to the support worker who returned Rachel to her care home.
3/
He ruled on a factual dispute, and found that on discharge Staff Nurse Kate Griffiths failed to provide a leaflet about dental surgery to the support worker who returned Rachel to her care home.
3/
The Coroner was satisfied that Rachel was fit to be discharged on the Friday evening after her surgery and that it was reasonable that she was.
Surgery was at 2pm and she was discharged at 7pm. She was awake, alert and singing before she left for home.
4/
Surgery was at 2pm and she was discharged at 7pm. She was awake, alert and singing before she left for home.
4/
The Coroner described unchallenged evidence that Rachel’s breathing was rattling or chesty on the Friday night and that she continued to bleed.
By 10:30am on Saturday Rachel was described as gurgling, with watery blood coming out of her mouth.
5/
By 10:30am on Saturday Rachel was described as gurgling, with watery blood coming out of her mouth.
5/
The qualified nursing staff working at Pirton Grange on the Friday night, Saturday day, Saturday night and Sunday morning failed to take more than one partial set of observations of Rachel
6/
6/
When they called 111 on Saturday evening they failed to provide adequate information to the out of hours nurse, who failed to sufficiently question when she return the call to them.
7/
7/
On the balance of probabilities she [OOH Nurse] should have asked direct questions about Rachel’s bleeding, what her chest sounded like, and what most her recent physiological observations had been. These were questions a trained health care professional should have asked.
8/
8/
The Coroner did not find Nurse Sheeba George to be a reliable witness.
As a matter of fact, on the balance of probabilities, I find Ms George did not take any physiological observations that evening, and that’s the reason she did not mention them in that phone call.
9/
As a matter of fact, on the balance of probabilities, I find Ms George did not take any physiological observations that evening, and that’s the reason she did not mention them in that phone call.
9/
The Coroner summarised the evidence relating to Rachel’s gradual decline, culminating in a 999 call and the arrival of paramedics shortly after 2pm on Sunday. Rachel had suffered an unsurvivable brain injury, as a result of her brain being starved of oxygen.
10/
10/
She received intensive care treatment in hospital before the decision was made to move her to end of life palliative care, when she was returned to her home at Pirton Grange, where she died on the 13 November 2018.
11/
11/
On the balance of probabilities, by Sunday, Rachel had already suffered some brain injury.
She should have been admitted to hospital on Saturday evening, and if she had been she probably would have survived.
12/
She should have been admitted to hospital on Saturday evening, and if she had been she probably would have survived.
12/
No doubt if Pirton Grange had in place a more robust system with policies, procedures, training and auditing, both those nurses would have carried out regular observations on Rachel over those two days, but that does not excuse their own failings.
13/
13/
Basic nursing checks should have carried out and recorded, their failure to do so meant anyone, including themselves trying to build a picture of how Rachel was faring in the hours after her surgery were being denied key pieces of information.
14/
14/
Coroner found the failure of the two nurses to carry out and document observations, and failure to seek emergency assistance from Saturday evening, amounted to a failure to provide basic medical attention to a person in a dependent position unable to provide it to herself.
15/
15/
He found each of those incidents so total and complete, so patently not a simple error, they cld only be described as a gross error.
16/
16/
He found the fact the Out of Hours Nurse did not ask sufficient questions was a failure ‘perhaps even a serious one, but not so serious as to amount to a gross failure’.
17/
17/
Coroner was satisfied if regular observations had been recorded, by Saturday evening they would have indicated the need for emergency assistance.
Had it been sought Rachel would have been relayed to hospital earlier, and the Coroner was satisfied she would have survived.
18/
Had it been sought Rachel would have been relayed to hospital earlier, and the Coroner was satisfied she would have survived.
18/
Therefore the two failures did contribute to Rachels’ death.
Short form narrative: Rachel died as a result of complications of necessary surgery, to which neglect contributed.
19/
Short form narrative: Rachel died as a result of complications of necessary surgery, to which neglect contributed.
19/
Coroner concluded: Mrs Johnston if I can address you directly, can I start by offering you and the rest of your family my sincere condolences for your loss. The description you’ve given of your daughter, one can only attempt to imagine the hole left in your life as a result.
20/
20/
Inquest is adjourned. Will resume on 23 February 2021 to hear the remainder of the Registered Manager of Pirton Grange’s evidence and to discuss Prevention of Future Deaths reports
/END
/END
• • •
Missing some Tweet in this thread? You can try to
force a refresh