What is a Groove Pancreatitis (GP)? #GroovePancreatitis #ParaduodenalPancreatitis #CysticDystrophyDuodenalWall What are the symptoms, consequences, management?
Do not miss this @aegastro #HiloAEG #UEGambassador @my_ueg Twitter thread #TheAmylaseSchool
Do not miss this @aegastro #HiloAEG #UEGambassador @my_ueg Twitter thread #TheAmylaseSchool

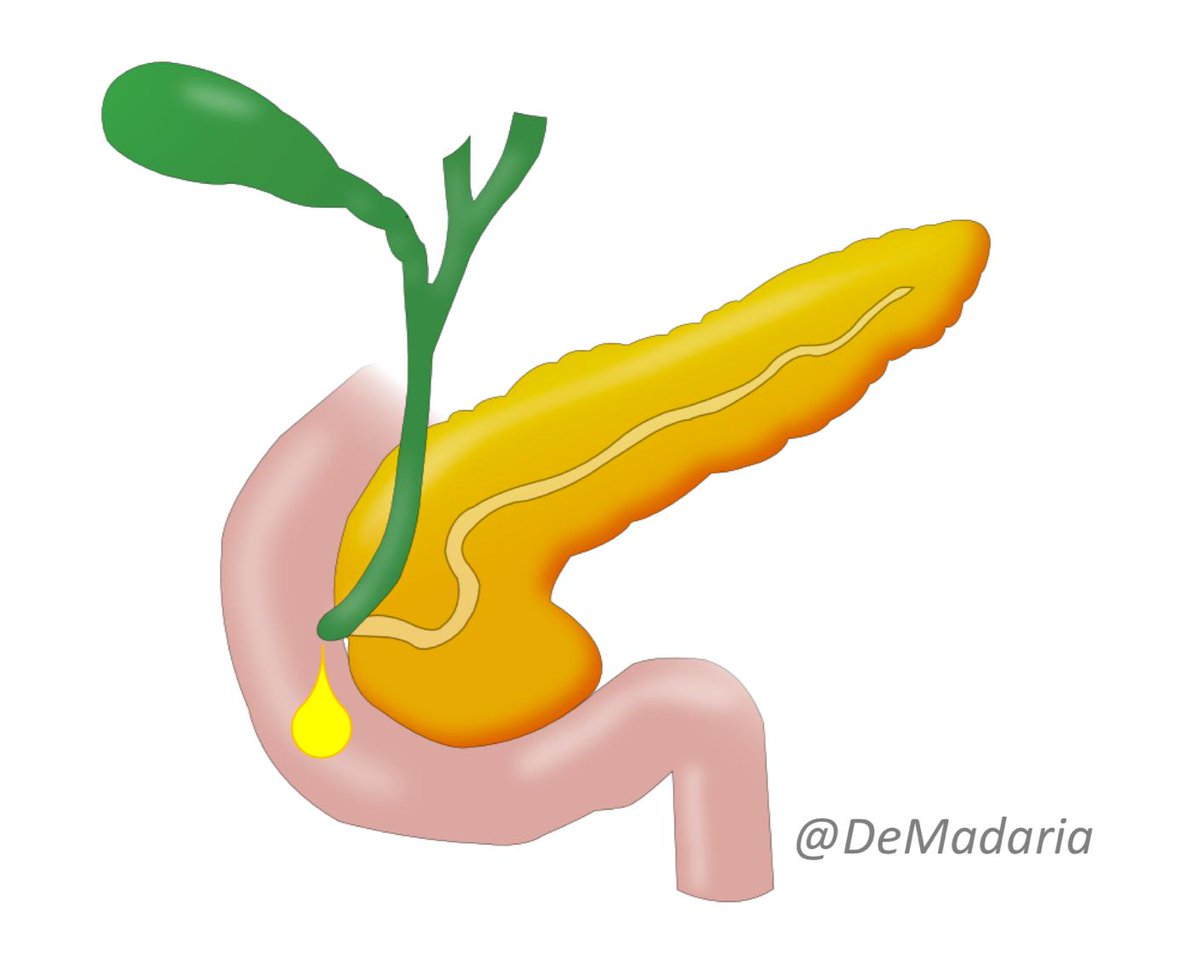
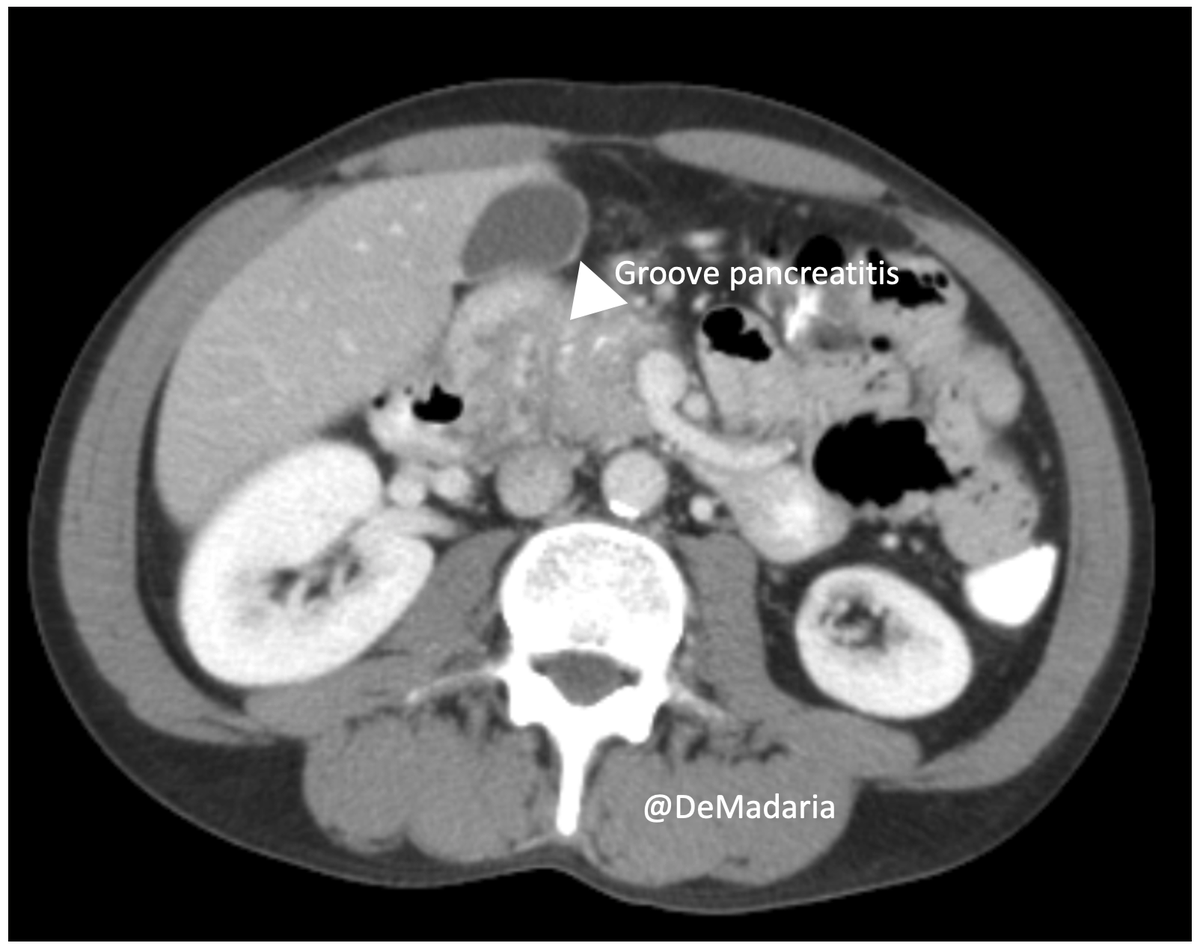
The groove area or pancreaticoduodenal groove involves the space between the duodenum, the head of the pancreas and the common bile duct karger.com/Article/FullTe… 

Groove pancreatitis is a segmental chronic pancreatitis that affects the groove area; it was described in 1973 by Becker
link.springer.com/book/10.1007/9…
link.springer.com/book/10.1007/9…

There are different names for this condition, some of them are specific conditions according to some authors: paraduodenal pancreatitis, cystic dystrophy of heterotopic pancreas, myoadenomatosis, periampullary duodenal wall cyst, and pancreatic hamartoma of the duodenum.
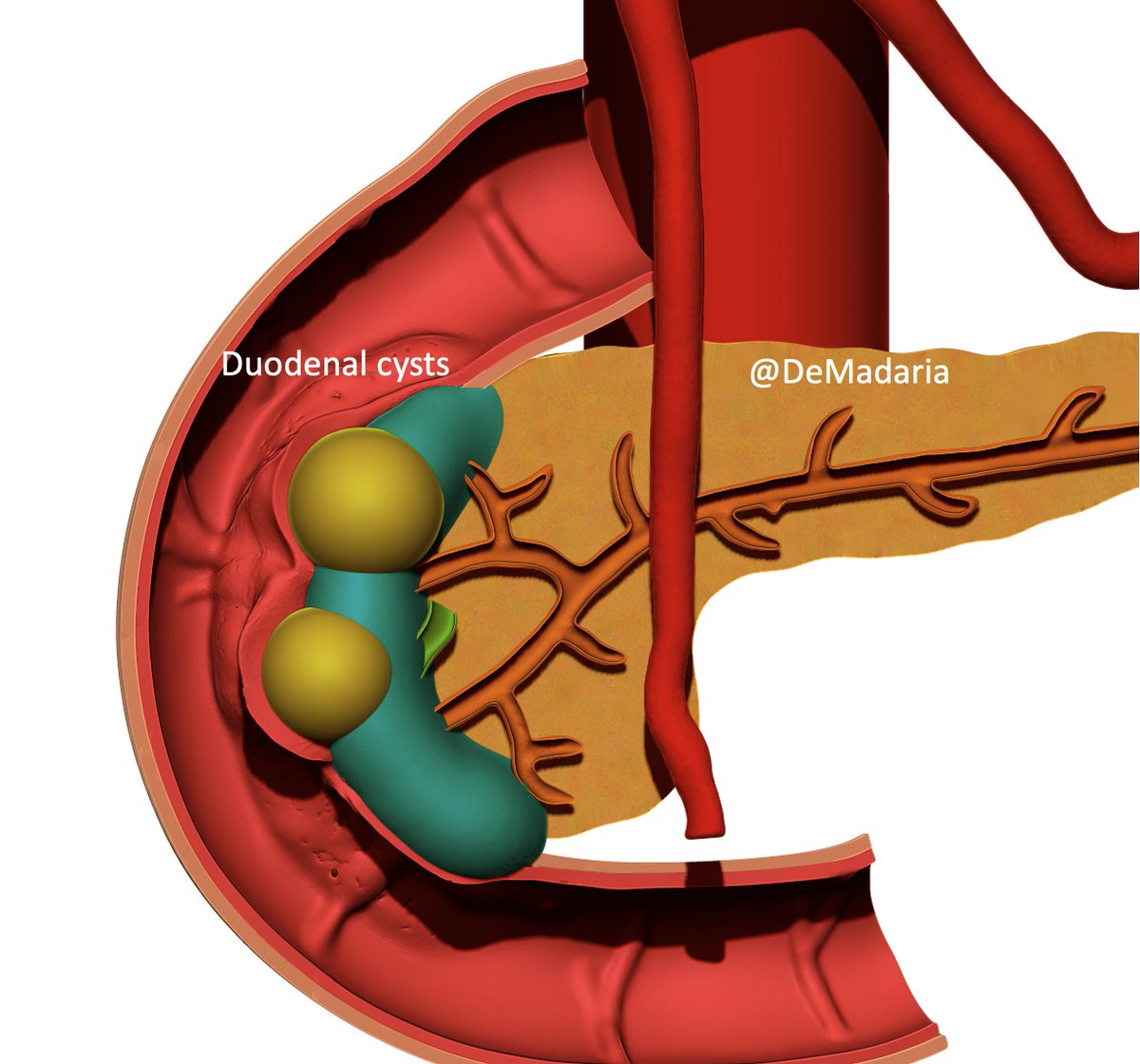
One special condition is cystic dystrophy of heterotopic pancreas: it involves duodenal wall inflammation and cysts due to inflammation of heterotopic exocrine pancreatic tissue of the duodenal wall. 




The most frequent etiology for GP is alcohol and tobacco (both in the literature and in my personal experience). For this reason the usual patient with GP is a male patient in the 4th-5th decade
According to a systematic review the median age of 47 years (range, 34 to 64 y), with 90% male, 87% smokers, and 87% alcohol consumption journals.lww.com/jcge/Abstract/…
GP may be associated to abdominal pain, duodenal obstruction and jaundice. It is frequently associated to typical signs and symptoms of chronic pancreatitis (calcifications, dilated main pancreatic duct…), and most patients have pancreatitis-like symptoms 


According to the systematic review, most patients presented with abdominal pain (91%) and/or weight loss (78%). Imaging frequently showed cystic lesions (91%) and duodenal stenosis (60%) journals.lww.com/jcge/Abstract/…
Treatment depends on symptom severity, response to conservative treatment and the development of complications. Endoscopy is an option in case of obstructive cysts, jaundice, but 1/3 patients initially treated by endoscopy are finally referred for surgery journals.lww.com/jcge/Abstract/…
Surgery is the most effective treatment with 80% complete symptom relief, but often conservative management and endoscopy are performed first journals.lww.com/jcge/Abstract/…
Thanks to @GVAsalualicante radiology and pathologic Departments for the images!
Now, what is your experience with groove pancreatitis?
Now, what is your experience with groove pancreatitis?
@KM_Pawlak @drdalbir @BilalMohammadMD @KralJan @drkeithsiau @MZorniak @DCharabaty @RashidLui @SunilAminMD @SanchezLunaMD @stevenbollipo @Samir_Grover @drmoutaz @RodriguezParra_
@liveRPancSurg @japariciot2 @Belenmm271 @lelecapurso @guspereztweets @tberzin @MendozaLadd @SWexner @almagoch @EdgardLozada @KMonkemuller @bisturitx @CMZavaletaMD @CabreraDacio @velardemd @Alxmd @ylseggrobe @e_santino @mauriciorincons @ferperezaguilar
@sanjay_HPB @NEndoscopy @JohnAGMoir @YouppiePancreas @hpb_so @HpbMo @OscarGuevaraHPB @manuknayar @elenamartin2222 @DerekAOReilly @jwindsor3 @ResearchSurgeon @oscarmazza
• • •
Missing some Tweet in this thread? You can try to
force a refresh