Sitrep: Yesterday marked a year since the first COVID-19 patient was admitted to @teamaccu @royallondonhosp. A year like no other. East London was badly hit by both the first and second waves. Many stories to tell. Here’s mine (long thread but easy read!). 1/22 

The four hospitals in @NHSBartsHealth has treated more than 8000 patients with COVID-19. This was beyond our wildest imagination a year ago. Even the worst winter ‘flu epidemic was tiny by comparison. The entire organisation forced to configure around a single disease. 2/22 

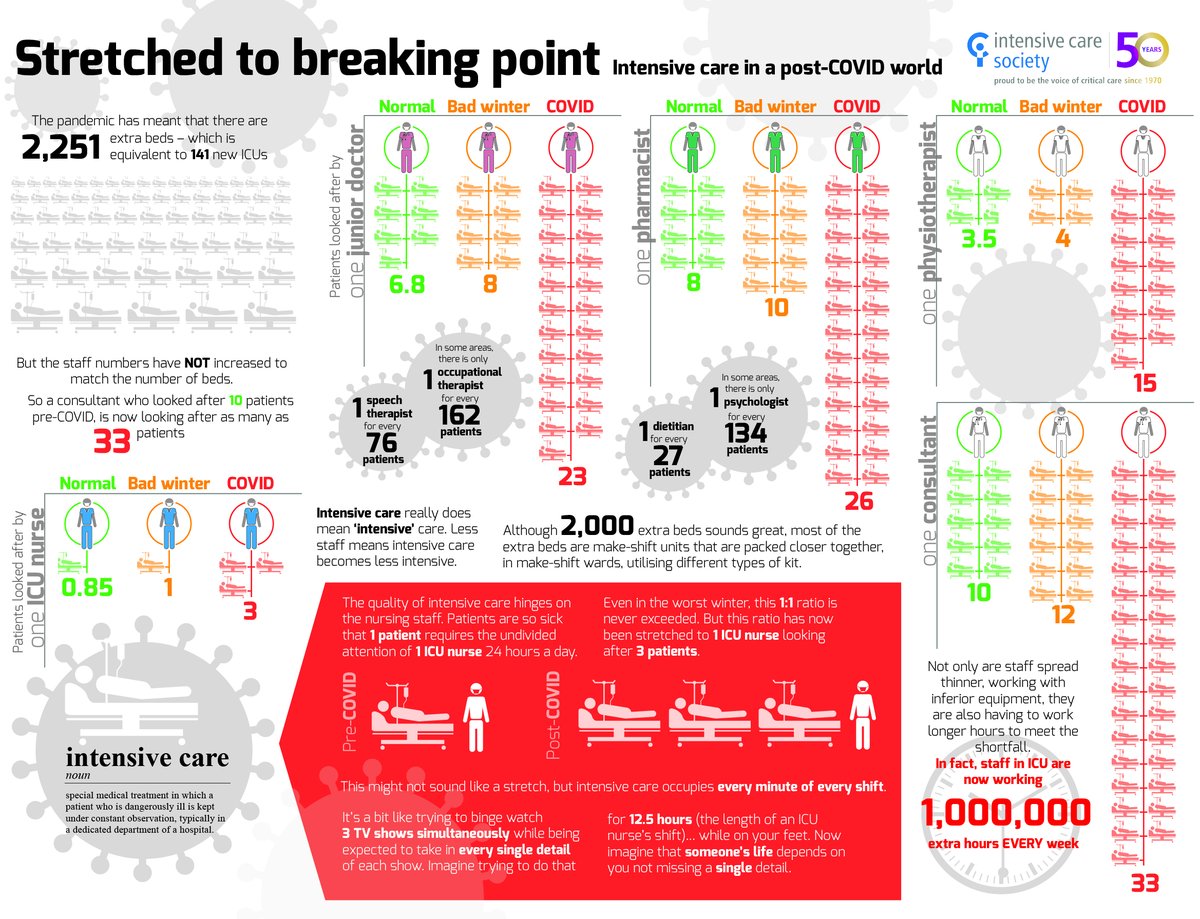
Our expanded @teamaccu has admitted 648 COVID patients in 12 months to an ICU which expanded three and a half times our original size to 150 beds. For ICU staff this is just mind boggling. An incredible logistical effort from staff of all grades from across @NHSBartsHealth. 3/22 

Early fears were of equipment shortages especially ICU ventilators. We were bombarded by inexperienced inventors trying to re-create these complex machines. It was madness, and a dangerous distraction. This excellent @BBCRadio4 programme explains why. 4/22 bbc.co.uk/programmes/m00…
But shortages of Personal Protective Equipment (PPE) were by far the most emotive issue. We had no idea how easily we could be infected or what the virus would do to us. Several NHS colleagues were admitted to hospital with COVID this year, and two to our own ICU. 5/22 

NHS Staff came to work with a genuine belief that they were risking their personal health. Glad to say I never had a situation where I did not feel I had the PPE to be safe. Our supply/logistics/manager colleagues made it their daily job to protect us. 💙 6/22 

We were beginning to understand what COVID-19 could do to a person. Of course, most cases are mild, but some are awful. 10-15% of hospital patients need ICU. Catastrophic lung damage often with kidney failure. Patient after patient, day after day, they kept coming. 7/22 

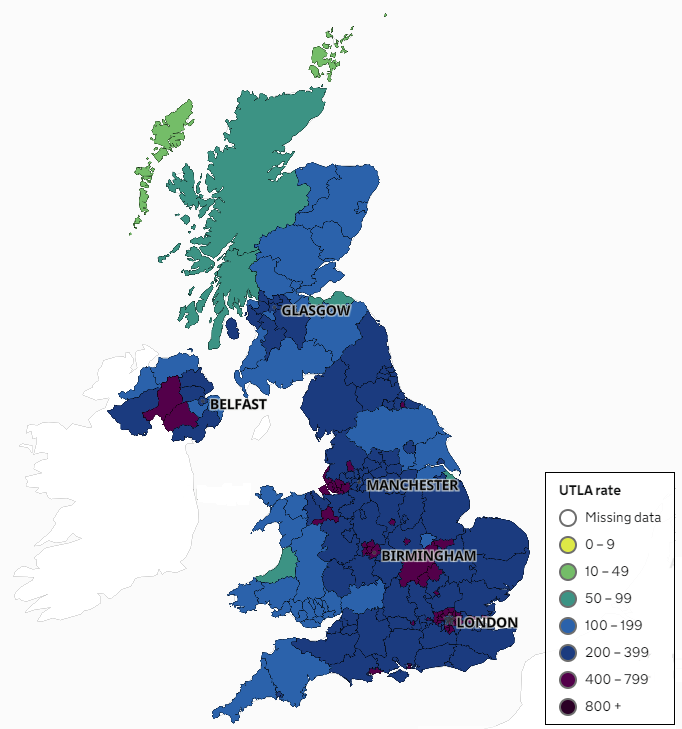
Patterns emerged. Ethnic minorities are more at risk of infection and more likely to die of COVID. Our local area was one of the worst affected in the UK. Tragic stories of deaths of everyday people filled the news. Very moving the first time everyone clapped on a Thursday. 8/22
There was a huge initiative to open ‘Nightingale’ Hospitals with the extra beds we feared we'd need. Many of us worried we might dilute the quality of ICU care so much that we'd end up with far more deaths. Doctors feared being held responsible. 9/22 bbc.co.uk/news/uk-englan…
Innovation mania also affected drugs. Every day brought news of a ‘cure’ for COVID. Hydroxychloroquine mysteriously sold out at high street pharmacists. Most theories were disproved in clinical trials. Only a few drugs saved lives eg dexamethasone. 10/22
bbc.co.uk/news/53559938
bbc.co.uk/news/53559938
By May things were pretty calm. We had opened a huge new ICU area on the 15th floor @royallondonhosp. We patiently treated the patients with lingering illness. By July many of us were taking well-earnt breaks. Some even managed a foreign holiday. 11/22 

Led by a few (non)experts, an aggressive COVID denial movement emerged. The false dichotomy: we must choose to protect the economy or protect our healthcare. Media reports of failings of NHS staff in the first wave. We felt the growing weight of impossible expectations. 12/22
October brought the madness of the ‘Great Barrington Declaration’. We watched COVID denial gather pace with anxious fascination. A 2nd wave was inevitable but we assumed it would be small. It began in October. We thought we had the measure of it…. 13/22 en.wikipedia.org/wiki/Great_Bar…
…we knew how to treat COVID. We had plans to increase ICU capacity, plenty of PPE and large numbers of ventilators ready to go. New infections reached a low peak in early November. A short loose lockdown ended. It was a false dawn. By December infections were rising fast. 14/22 

The rapid rise of the true second wave was genuinely frightening: (a) we didn’t know when it would stop and (b) COVID denial was everywhere. Doctors were accused of faking deaths in a global conspiracy. Others did everything they could to undermine public health measures. 15/22
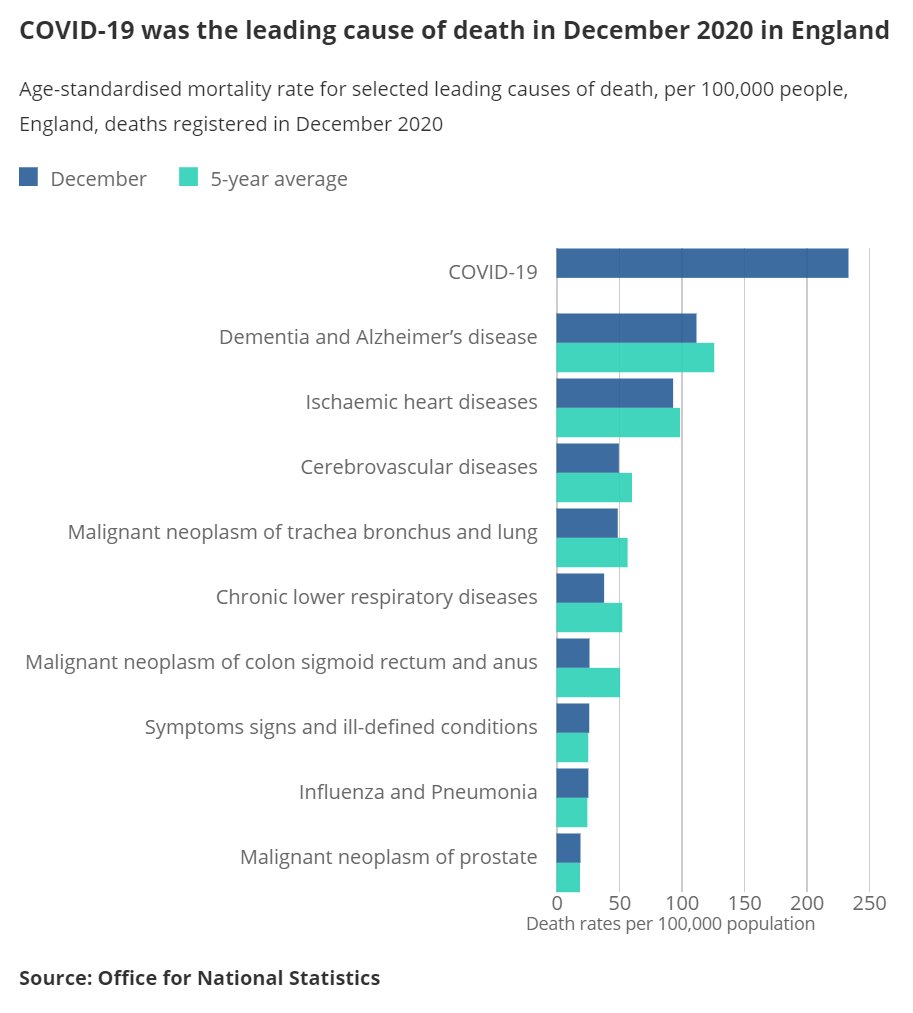
Once again, we had no idea how high the peak would be. The nation pored over daily graphs of rising case numbers. Was COVID really that bad? Was it any worse than ‘flu? There was a national debate between saving Christmas and saving the NHS. 16/22
news.sky.com/story/covid-19…
news.sky.com/story/covid-19…
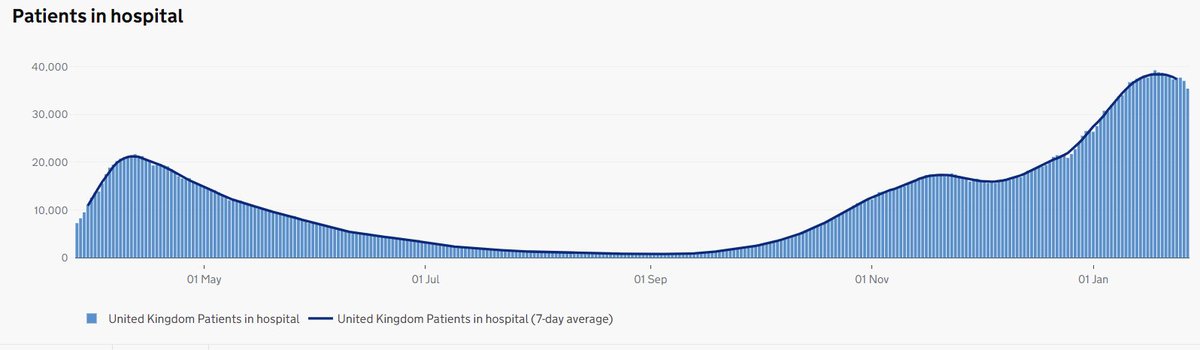
We knew hospital admissions lagged behind new infections by about a week, and ICU admissions a few days after that. We obsessed over the stats on a daily basis looking for infections to peak. Every stutter in the numbers was a worry (we had been caught out in November)… 17/22
…and we did constant mental arithmetic on how many more ICU beds we could find, how much further our ICU staff could stretch, and how many more days the rise would continue. The deniers began to fall silent. Not a good sign. Vaccines arrived just after Christmas.💙18/22
New cases actually peaked on 6th January, hospital admissions on the 12th, and ICU admissions on 23rd Jan. But it wasn’t until 30th Jan that I felt confident we had reached the high water-mark for the second wave. Two months of dreadful worry. 19/22
https://twitter.com/rupert_pearse/status/1355424710796959745?s=20
The second wave is/was really hard. NHS staff are now very tired. Morale was badly undermined by the lockdown debate. But as the numbers rose, staff kept digging deeper and deeper. Senior doctors volunteered to help in ICU nursing roles. Everyone pitched in. 20/22 

So much learning; where to start? My two penneth: The waves of infection will continue until we take the virus seriously. There seems no limit to what NHS staff will do to keep their patients safe. Many were prepared to die in harness. We cannot let this happen again. 21/22
This year would have been so much worse without the common sense and team spirit of many millions of people. You stuck to the rules. You cheered us on. You sent supplies with messages of kindness and support. We are proud to be your NHS.💙 22/22 

• • •
Missing some Tweet in this thread? You can try to
force a refresh