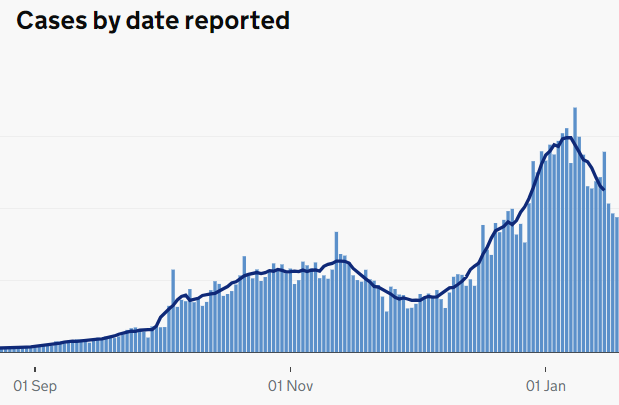
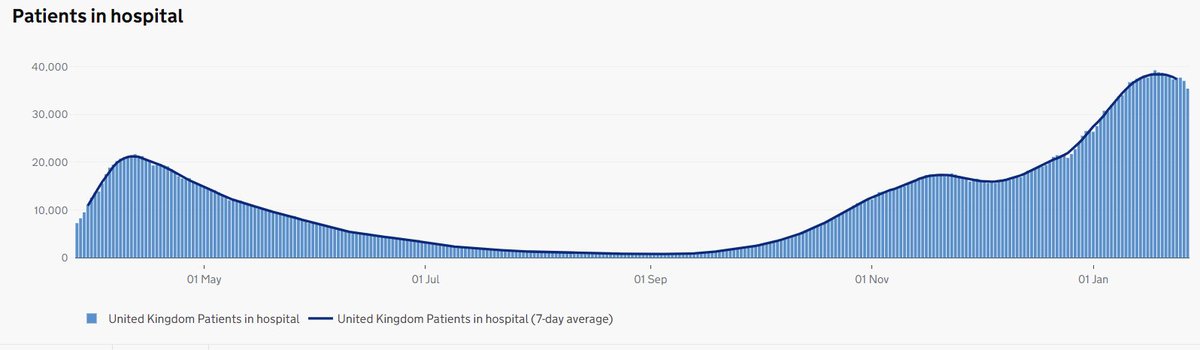
Sitrep: situation report. This is what we call our daily briefings right now. Here’s mine. We are now fairly confident we have reached the high water-mark for the second wave of COVID-19 NHS hospital admissions across the UK. Good news but.... 1/10 
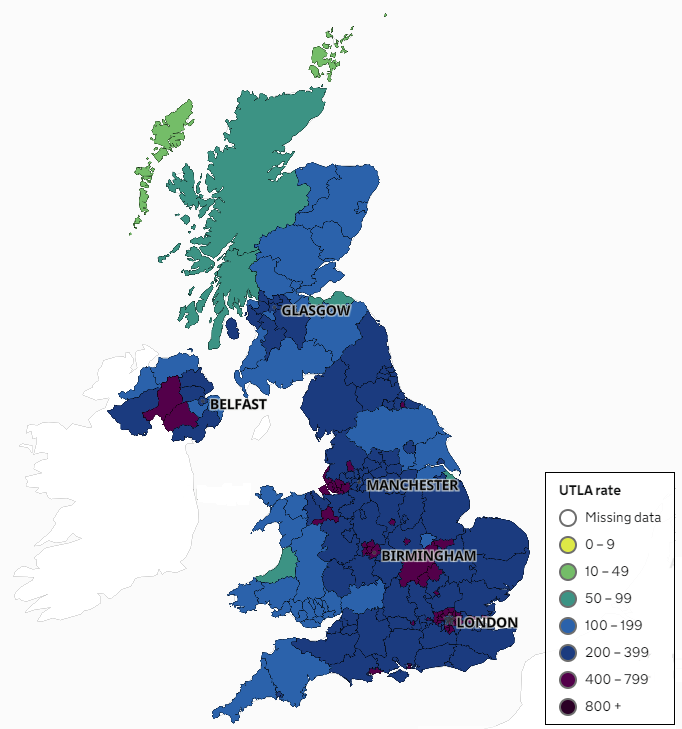
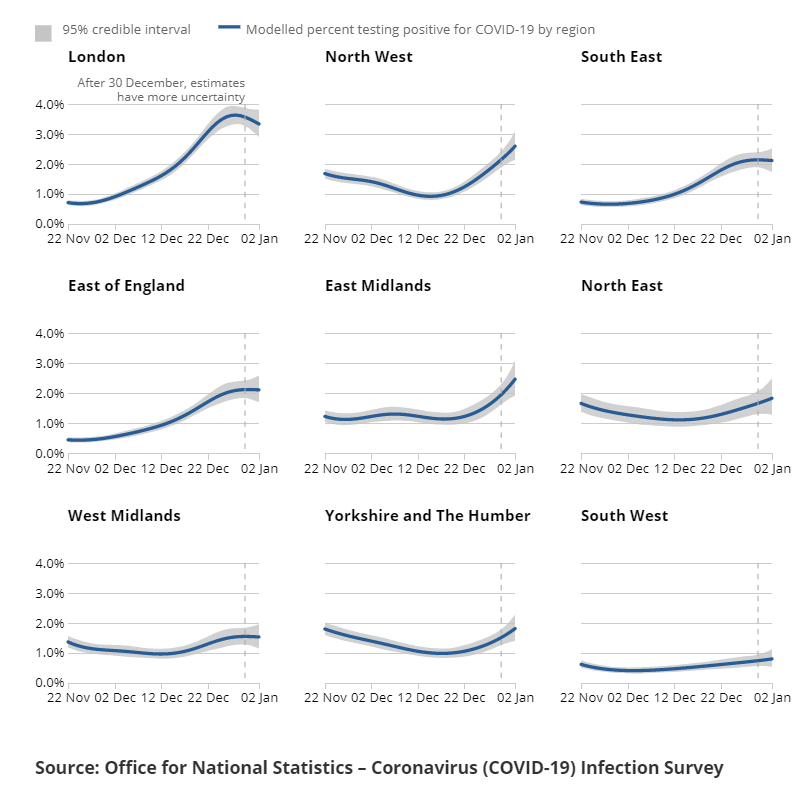
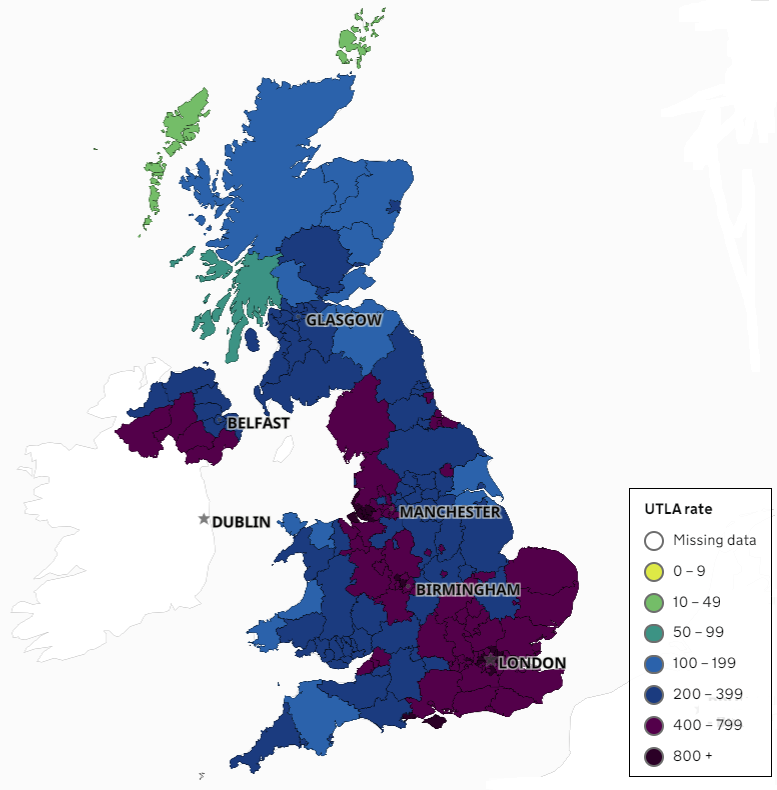
....we still have nearly 40,000 patients in hospitals with COVID-19. Despite huge increases in staffing, we are very short-handed. In many hospitals, admissions have stabilised but not all. Some differences across the UK. Things still getting worse in the Midlands and North. 2/10 
4000 of these patients (10%) need intensive care. This is huge: in January 2020 the UK had only 4100 adult ‘critical care’ beds including both ‘intensive care’ ventilated beds for the sickest patients and 'high dependency' beds for less sick patients. 3/10
kingsfund.org.uk/publications/c…
kingsfund.org.uk/publications/c…
This is important because sceptics have spread deliberate misinformation about ICU ‘occupancy’ to obscure massive increases in ICU capacity. Ensuring we have a bed for every patient means we must have empty beds ready to admit them to ICU urgently. 100% occupancy isn't good. 4/10
Our usual strict rule of one trained nurse for each intensive care bed has been stretched to 1:3 and in many hospitals, to 1:4. We are still filling these gaps with nurses from other departments, retired nurses, medical students, and hospital consultants (senior doctors). 5/10 

So while the situation is becoming less serious we cannot relax. The quality of patient care is not the same as usual and many other routine NHS services have given up staff to care for COVID patients. The care of patients with less urgent illnesses is still badly affected. 6/10
But mostly we can stop planning for further increases in patient numbers and focus on consolidating our response. We can think much more about the quality of patient care and how we can improve it. We are starting to look at longer term planning for COVID. 7/10
Sadly, COVID is here to stay. We will still have lots of COVID patients in hospitals in June. We must plan for winter COVID crises just as we did for winter flu epidemics. COVID will become endemic (present at low levels) and gradually take its place in the NHS routine. 8/10
On the plus side, we now understand this disease really well. We will know how to prevent and control future COVID epidemics and how to anticipate the need for NHS capacity. We will get better and better at keeping usual NHS care going while we respond to smaller outbreaks. 9/10
Meanwhile, following public health guidance remains vital to protect everyone’s healthcare. Please keep up your amazing work with #HandsFaceSpace. Politely call out those who question the need, especially public figures with big audiences. This will help save lives. 10/10 💙 

• • •
Missing some Tweet in this thread? You can try to
force a refresh