Slogans aside, there are three broad approaches to COVID countries can take from now on:
A. An R<<1 approach
B. An R<1 approach
C. An R>1 approach
Let's break them down... 1/
A. An R<<1 approach
B. An R<1 approach
C. An R>1 approach
Let's break them down... 1/
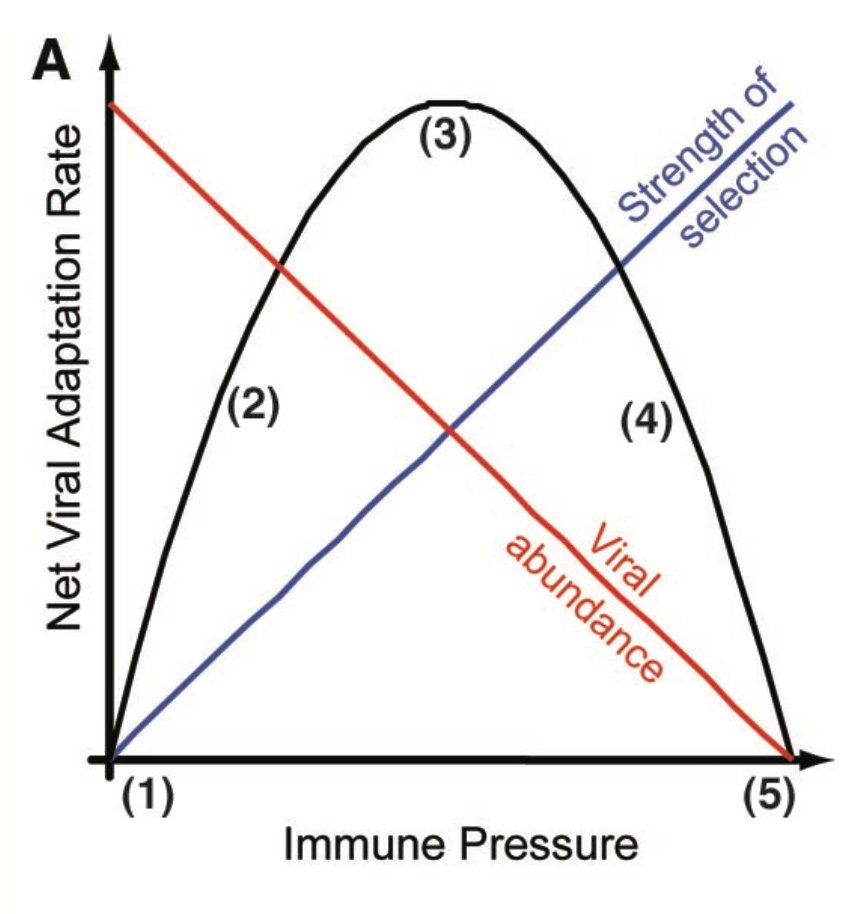
A. An R<<1 approach means keeping R as low as possible with stringent measures until no local transmission. E.g. this is what Auckland and Melbourne did recently in response to a handful of new cases. 2/
B. An R<1 approach means keeping epidemic declining, although transmission may still continue for a long time as measures are relaxed. As coverage increases, vaccination could also 'buy' some additional reduction in R & allow more reopening under such an approach. 3/
C. An R>1 approach in the era of vaccines means relaxing measures to point where there could be some rise in infection, but with cases eventually declining either because vaccine protects sufficiently against disease, or because additional natural immunity has accumulated. 4/
The effort required to follow each approach - and corresponding epidemic impact - will obviously depend on vaccine characteristics, coverage, and current local infection prevalence. But I think these categories are useful to define what people are actually talking about. 5/5
• • •
Missing some Tweet in this thread? You can try to
force a refresh