
1/ How much does "Dietary Cholesterol" impact blood cholesterol levels?
This has been making the rounds lately and I have an experiment from 2018 is key to this question 👇
Remember the "White Bread and Processed Meat" experiment? cholesterolcode.com/the-tandem-dro…
This has been making the rounds lately and I have an experiment from 2018 is key to this question 👇
Remember the "White Bread and Processed Meat" experiment? cholesterolcode.com/the-tandem-dro…
2/ If you've followed me a while, you know I believe it isn't the actual ingestion of cholesterol on #LowCarb that has a big impact on serum levels -- it's predominantly the trafficking of fat. (See CholesterolCode.com/model)
But this is actually a very testable distinction...
But this is actually a very testable distinction...
3/ All we need is an experiment where I consume a lot of (1) low fat food that still (2) has ample amounts of cholesterol.
Thus, the "processed meat" side of the experiment is key if it has a decent amount of cholesterol -- and it does.
For example 9/21/18 I ate the following..
Thus, the "processed meat" side of the experiment is key if it has a decent amount of cholesterol -- and it does.
For example 9/21/18 I ate the following..
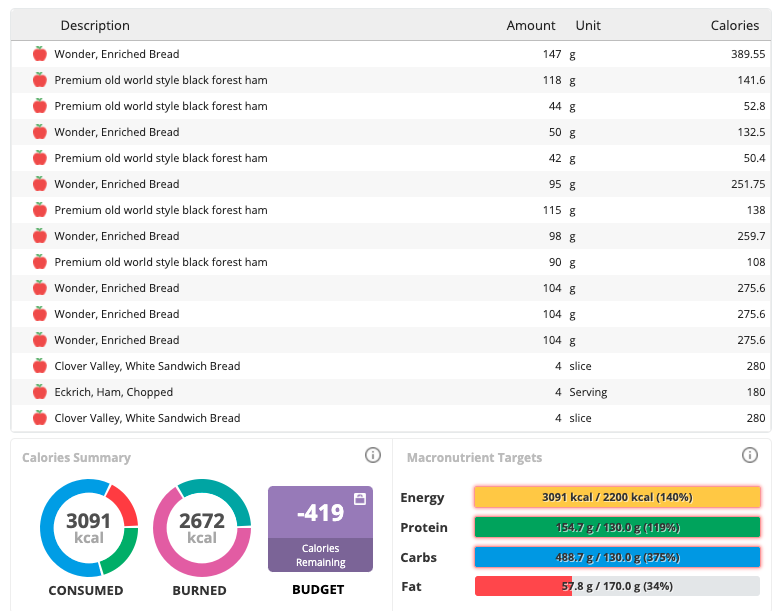
4/ 409g Land O' Frost Premium Old World Style Black Forest Ham
- and -
113g Eckrich Chopped Ham
... Come to 265mg of cholesterol.
On the morning of that day my Total and LDL cholesterol were 317 and 233 respectively. So what happened as I continued to eat this way for 7 days?
- and -
113g Eckrich Chopped Ham
... Come to 265mg of cholesterol.
On the morning of that day my Total and LDL cholesterol were 317 and 233 respectively. So what happened as I continued to eat this way for 7 days?
5/ ...My Total and LDL cholesterol levels were dropping substantially
Again, I think there are many reasons for this I discuss frequently with the #LipidEnergyModel
But the point of this thread is to demonstrate how much (or rather, how little) dietary cholesterol mattered
Again, I think there are many reasons for this I discuss frequently with the #LipidEnergyModel
But the point of this thread is to demonstrate how much (or rather, how little) dietary cholesterol mattered

6/ It's worth adding that there's some biochemistry that helps potentially explaining much of this. Most cholesterol we ingest is in the form of esters which commonly pass through our digestive tract, yet most cholesterol in our blood was actually made by our liver "de novo"
7/ Moreover, I learned early on from Dayspring's lectures the body compensates depending on ingestion. Generally speaking, if you have less coming in from the diet, the body makes more and vice versa.
I should probably tag @lowcarbGP as he's been talking about this lately as well...
• • •
Missing some Tweet in this thread? You can try to
force a refresh



