1/ Thread ➡️This is a good spot to remind everyone why @DrNadolsky, @DrRagnar and I are doing the #LMHRstudy
(@nicknorwitz, I'm going to use you as an example, if you don't mind)
Nick has an LDL-C of 521, well into range of Homozygous Familial Hypercholesterolemia (HoFH)...
(@nicknorwitz, I'm going to use you as an example, if you don't mind)
Nick has an LDL-C of 521, well into range of Homozygous Familial Hypercholesterolemia (HoFH)...
https://twitter.com/nicknorwitz/status/1370717112721870848
2/ FH, particularly HoFH is highly associated with atherosclerosis and is considered a substantial risk.
Cases of HoFH are extremely rare, but are considered a cornerstone of the lipid hypothesis as many with LDL-C levels (comparable to Nick's) demonstrate CVD as children...
Cases of HoFH are extremely rare, but are considered a cornerstone of the lipid hypothesis as many with LDL-C levels (comparable to Nick's) demonstrate CVD as children...
3/ Brown and Goldstein have seminal work on this topic.
In particular, this is worth reading in regard to this subject: ncbi.nlm.nih.gov/pmc/articles/P…
(Warning: this includes many graphic images of xanthomas, which are more common with high LDL FH)
In particular, this is worth reading in regard to this subject: ncbi.nlm.nih.gov/pmc/articles/P…
(Warning: this includes many graphic images of xanthomas, which are more common with high LDL FH)
4/ "The early atherosclerosis in homozygous FH children who do not have any other risk factors (e.g., smoking, hypertension, diabetes, type A personality) provides formal genetic proof that elevated LDL alone can produce atherosclerosis in humans."
5/ While it's true that I'm "cautiously optimistic" with regard to higher LDL-C / ApoB in the context of metabolic fat adaptation (see below), I'm by no means certain.
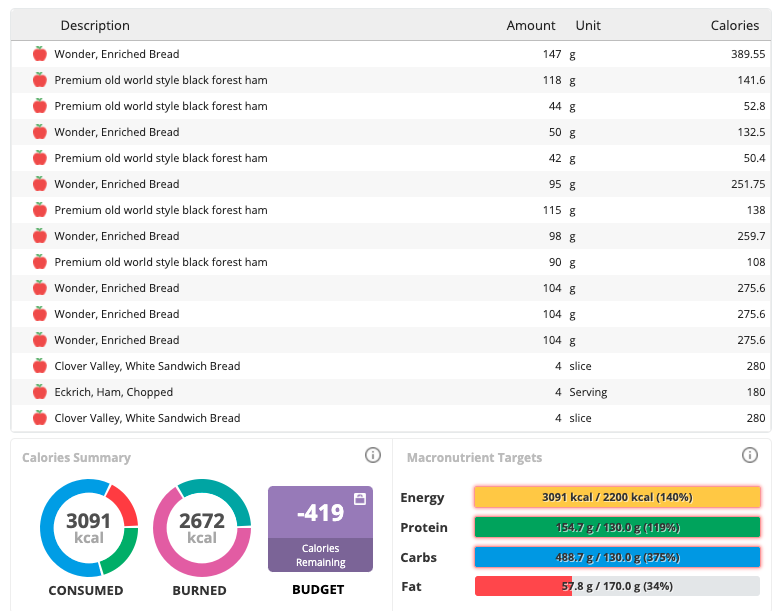
I'm not just waxing philosophic. I have LDL-C at 1/2 of Nick's on #keto at ~250 mg/dL
CholesterolCode.com/model
I'm not just waxing philosophic. I have LDL-C at 1/2 of Nick's on #keto at ~250 mg/dL
CholesterolCode.com/model
6/ As always, I point to the set of clues on metabolic fat adaptation that (I hypothesize, per the model) typically results in high HDL and low TG that we see in this phenotype, the so called "Lipid Triad" (Triad) of ⬆️LDL+⬆️HDL+⬇️TG.
But I won't go into detail on that here...
But I won't go into detail on that here...
7/ Just note we are not outliers. At the CC site, CC and LMHR Facebook groups, and recent surveys like (
https://twitter.com/DaveKeto/status/1320418456353697792?s=20) I can say with confidence there are *at least* tens of thousands with LDL ≥ 200, and *at least* over a hundred with LDL ≥ 500 (w/ ⬆️HDL+⬇️TG).
8/ So let me restate this for extra emphasis: We don't know if this population is at considerable risk for atherosclerosis.
When I say I'm "cautiously optimistic", don't read as "completely certain"- or I wouldn't be working so hard to help gather key data, such as this study
When I say I'm "cautiously optimistic", don't read as "completely certain"- or I wouldn't be working so hard to help gather key data, such as this study
9/ For better or for worse, the LMHR phenotypes afford a uniquely distinctive population for testing the exposure of interest (LDL-C/ApoB) in the absence of other major CVD risk factors to better confirm it's independent atherogenicity.
• • •
Missing some Tweet in this thread? You can try to
force a refresh