Hi #IDFellows and #IDTwitter, back with another case: 63F h/o ESRD on HD p/w fever. Blood cx positive for MSSA x 4 days. Blood cx clear on day 5 with Rx Cefazolin. TTE on HD2 without vegetations. What is the best next step?
1/ Let’s talk about when to get a TEE for Staph aureus bacteremia (SAB) to identify infective endocarditis (IE)!
This is a #IDControversy for #IDFellows & #IDTwitter. Let's examine the evidence.
This is a #IDControversy for #IDFellows & #IDTwitter. Let's examine the evidence.
2/ For background, SAB has a high mortality (~20%); determining the presence of IE changes the duration of treatment to 6+ weeks.
The sensitivity of TTE for IE is ~60-65% compared to ~95% for TEE. But TEE has associated costs & procedural risks (sedation, esophageal perf, etc)
The sensitivity of TTE for IE is ~60-65% compared to ~95% for TEE. But TEE has associated costs & procedural risks (sedation, esophageal perf, etc)
3/ A review of SAB literature in 2014 found 9 very low to low quality studies assessing the role of echocardiography for SAB. TTE poorly predicted presence of TEE results (15-19% of negative TTEs had IE on TEE).
pubmed.ncbi.nlm.nih.gov/25268440
pubmed.ncbi.nlm.nih.gov/25268440
4/ In this study, these criteria identified patients at low risk for IE from SAB (NPV 93-100% in 5 studies):
1) No permanent intracardiac devices
2) Follow-up BCx negative within 4 days
3) Not on HD
4) Nosocomial SAB
5) No secondary foci of infection or clinical signs of IE
1) No permanent intracardiac devices
2) Follow-up BCx negative within 4 days
3) Not on HD
4) Nosocomial SAB
5) No secondary foci of infection or clinical signs of IE
5/ Using a high quality TTE in a lower risk patient could preclude use of TEE using “strict negative criteria” for TTE interpretation. Using this criteria, a strict neg TTE has a NPV of 97.1%. However, only 26% of patients in this study had SAB.
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…

6/ A series of prediction tools using retrospective data have been developed, namely the PREDICT score from @MayoClinicINFD & the VIRSTA score from France
PREDICT: pubmed.ncbi.nlm.nih.gov/25810284
VIRSTA: pubmed.ncbi.nlm.nih.gov/26916042
PREDICT: pubmed.ncbi.nlm.nih.gov/25810284
VIRSTA: pubmed.ncbi.nlm.nih.gov/26916042
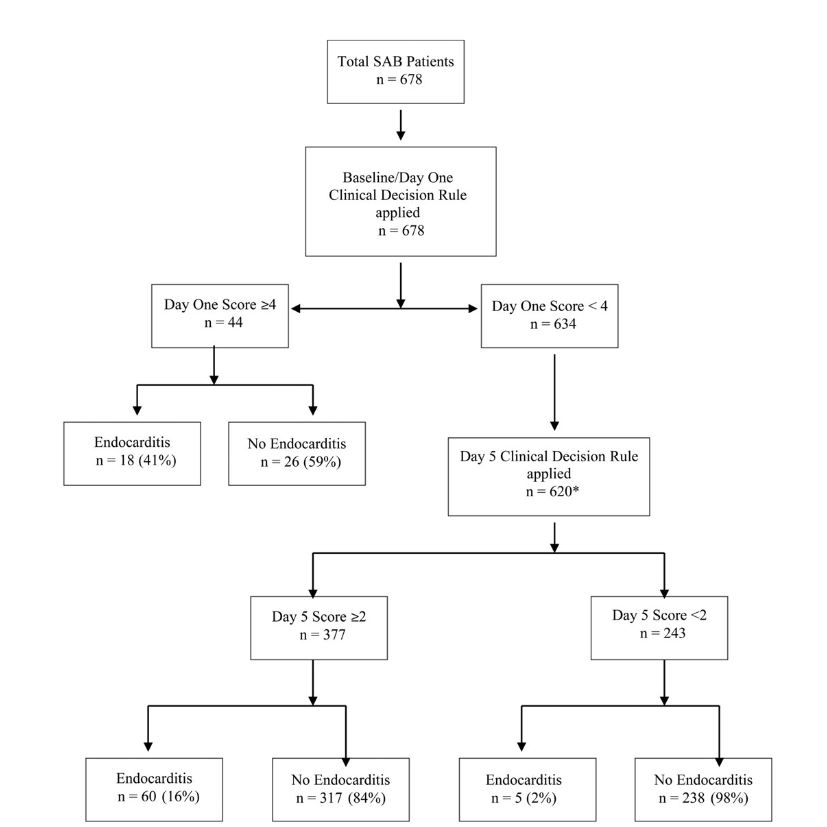
7/ In PREDICT, points were assigned on day 1 & 5 as follows:
ICD➡️2, PPM➡️3, community-onset➡️2, healthcare-associated➡️1, bacteremia≥72h➡️2.
Day 5 score <2 was 98.8% sensitive with a 98.5% NPV for IE. Need for TEE ⬇️35%.
But, all with community-acquired SAB require TEE.
ICD➡️2, PPM➡️3, community-onset➡️2, healthcare-associated➡️1, bacteremia≥72h➡️2.
Day 5 score <2 was 98.8% sensitive with a 98.5% NPV for IE. Need for TEE ⬇️35%.
But, all with community-acquired SAB require TEE.
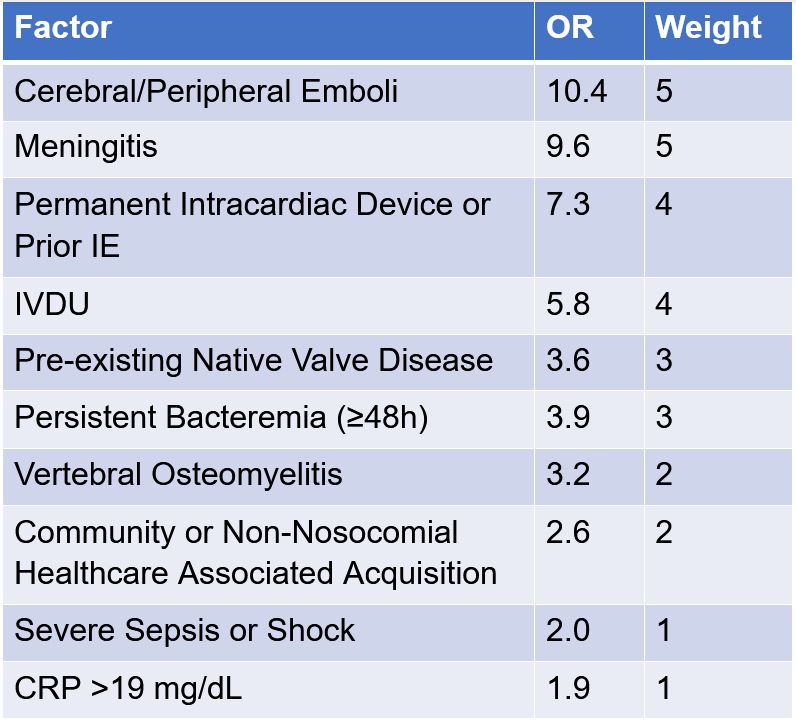
8/ VIRSTA included 2008 patients with SAB & found 10 weighted variables associated with IE in first 48 hrs.
A score ≤2 had a sensitivity of 95.8% with a NPV of 98.8%, so a score ≥3 should prompt TEE eval. Nearly 40% ⬇️ in TEE utilization.
A score ≤2 had a sensitivity of 95.8% with a NPV of 98.8%, so a score ≥3 should prompt TEE eval. Nearly 40% ⬇️ in TEE utilization.
9/ In Feb 2021, the external validity of PREDICT & VIRSTA was performed in 922 patients with SAB in Columbia.
academic.oup.com/cid/advance-ar…
academic.oup.com/cid/advance-ar…
10/ A negative VIRSTA score had a sensitivity of 96.7% with NPV of 99.5%.
Comparatively, a negative day 5 PREDICT score was only 51.6% sensitive with NPV of 95.1% & missed 4.8% of cases of IE (vs 0.44%).
A negative VIRSTA avoided 49.2% of TEEs.
Comparatively, a negative day 5 PREDICT score was only 51.6% sensitive with NPV of 95.1% & missed 4.8% of cases of IE (vs 0.44%).
A negative VIRSTA avoided 49.2% of TEEs.

11/ Neither PREDICT or VIRSTA have a high specificity or PPV at assigned cut-offs, but they have utility in determining low-risk patients to avoid invasive TEE testing.
Further studies are needed & defined utility of other modalities (e.g., PET-CT) still need to be elucidated.
Further studies are needed & defined utility of other modalities (e.g., PET-CT) still need to be elucidated.
12/ How do YOU make the decision about which patients get TEE in SAB? Do you prefer one of the scoring systems to the other?
13/ Thanks for tuning in #IDFellows and #IDTwitter! This Tweetorial was brought to you by the always amazing, @JonathanRyderMD!
If you are interested in contributing to @ID_fellows, let us know! And don't forget to checkout @IDFellowsCup for information on our upcoming game!
If you are interested in contributing to @ID_fellows, let us know! And don't forget to checkout @IDFellowsCup for information on our upcoming game!
@wuIDq @BIDMC_IDFellows @Tufs_ID @IUIDfellowship @UAB_ID @yaleIDfellows @ID_musc @templeID1 @VUMC_IC @MayoclinicINFD @MGH_ID @UCLA_ID @MontefioreID @UNMC_ID @UVA_ID @OhioState_ID @UTSWinfDis @BrownIDprogram @RushCCH_ID @OHSU_ID
• • •
Missing some Tweet in this thread? You can try to
force a refresh