What is “Bloodburn”? In the @starwars Universe, this mysterious chronic hematologic condition led Greer Sonnel - Senator Leia Organa’s chief of staff - to quit spaceship racing. #HematologyTweetstory 36: hematologic changes from space travel, in fantasy & reality. Image:@NASA/1 

First, some sci-fi fun. #StarWars fandom source “Wookipedia” (@WookOfficial, source of below image) tells us Bloodburn is a “rare, chronic, and often terminal illness of the blood that befell (often younger) starship pilots”. Symptoms include fevers... /2 starwars.fandom.com/wiki/Bloodburn 

Bloodburn is incurable, but usually manageable with good diet, hydration, rest, & “hadeira serum” injections (the serum itself can be harmful). The pathophysiology of Bloodburn is unclear. The “burn” part suggests radiation mediated-injury, but maybe just refers to the fevers?/3 

Curiously, the @StarTrek Universe includes a condition with a similar name: “Symbalene blood burn.” This highly contagious disease kills within minutes. Samples of the causative agent were stored on an asteroid (Cold Station 12) for research. memory-alpha.fandom.com/wiki/Symbalene… /4 



Space-originating but closer to home: the peculiar alien microorganism in Michael Crichton’s “Andromeda Strain” (1969 novel & 1971 film) caused rapid thrombosis. It was a weird & highly mutable crystalline organism lacking DNA, RNA, and proteins./5 



Human infection by the anerobic rod-shaped bacteria “Bacillus Vampiris” in Richard Matheson’s 1954 novel “I am Legend” caused a lust for blood, treatable with a pill containing dehydrated blood. The Will Smith film @iamlegend changed the causative agent into an measles virus./6 



In 2007, when the Will Smith film came out, I was @MayoClinic where hematologist Stephen Russell, Kah-Wye Peng & myeloma colleagues @VincentRK were doing early clinical trials w/ an oncolytic measles virus. A recent summary of that field in @nature: nature.com/articles/d4158… /7
Needless to say, the idea that a therapeutic virus might somehow turn patients into bloodthirsty zombies was not really the sort of publicity they were looking for. At least the IRB did not require this SAE in the informed consent. Image: Russell SJ, Peng K-W Mol Therap 2017 /8 

Another mysterious fatal blood illness: whatever Jenny Cavilleri had in 1970’s “Love Story”. It apparently caused the victim to both become more beautiful as the disease advances & generate vapid platitudes, such as “Love means never having to say you’re sorry.”🤮But I digress./9 



So what happens to *real* humans in space? Since the 1960s, there have been a number of studies of the hematologic changes associated with orbital flight. Not surprisingly, the effects of long-term missions may vary from those of short-term missions. (Image: @Medscape /ASGSB)/10 

The effects of VERY long term journeys, like Earth-to-Mars travel, are not yet entirely known, but there has been a lot of research into what *might* happen, and ways to mitigate potential disasters./11 

Space is brutal. Our bodies aren't designed for microgravity, or the ionizing radiation levels outside of the shielding atmosphere. The emotional toll of isolation (cue David Bowie's “Space Oddity”), prolonged confinement in small places, & distance from Earth can be tough./12 



@NASA’s Human Research Program has focused on understanding these physical and psychological risks for more than 50 years. nasa.gov/hrp /13
Early hematology studies done on 6 astronauts on Gemini missions in the 1960s (Gemini IV w/ White & McDivitt, V w/ Cooper & Conrad, VII w/ Apollo 13 hero Lovell & Borman who got his name on a major expressway in Indiana) included CBCs and radiolabeled red cell mass assessment./14 







The Gemini analyses indicated decreased hemoglobin levels and reduced red blood cell mass in all returning astronauts, as described in a classic 1967 @jama paper by Craig Fischer (now a retired space consultant) & colleagues. This led to similar studies in the Apollo program./15 



Studies of astronauts on Skylab missions in the 1970s included analysis of RBC metabolism and morphology, immune cell subsets, & conventional cytogenetics. Lots of vintage instruments are depicted on @NASA Life Sciences page for 1973 Skylab 2 mission: lsda.jsc.nasa.gov/Mission/miss/40 /16 



Despite 100% oxygen in the spacecraft cabin, hemoglobin & hematocrit were consistently low in returning astronauts. Terms like "astronaut anemia" and "anemia of spaceflight" were coined to describe these change, as in this 1984 classic by Mehdi Tavassoli, then in Boston. /17 



Some of this "anemia" was believed to be due to plasma volume changes: i.e., central/cephalad redistribution of ~2L of blood, which drops plasma volume by 10%... and which then shifts back upon return to 1g on Earth, diluting RBCs. (Image: Medscape/ASGDB) /18 

The Soviets were doing blood studies on their cosmonauts, with similar findings. There was very little sharing of information between space programs during the Cold War, but some publications from the USSR like this one did make it to the West & were translated for @NASA use./19 



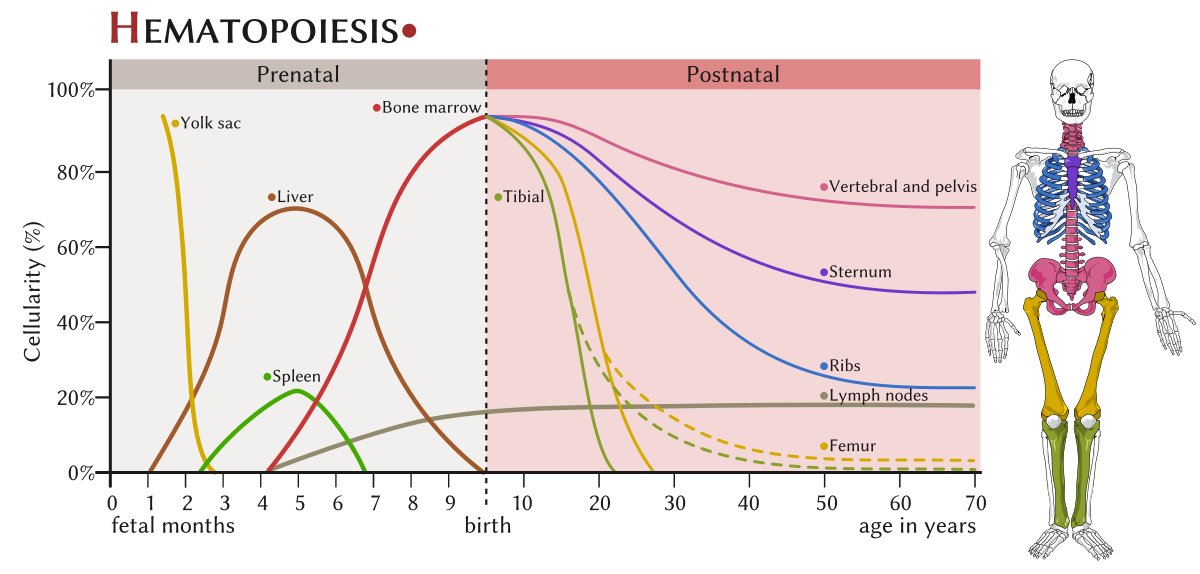
In the 21st century, the phenomenon of “neocytolysis” - i.e., selective hemolysis of the youngest circulating red blood cells upon perceived polycythemia – was postulated to be a contributor to space anemia, and also a more nuanced view of the plasma volume changes emerged./20 






More recently, the idea that space flight consistently results in anemia has been challenged. One criticism of the early studies from the Gemini-Apollo-Skylab era is that the RBC measurements were always done once the astronauts returned to Earth. space.com/38877-astronau… /21 

Hawley Kunz @NASA, Richard Simpson @UHouston & colleagues looked at whole blood from 31 astronauts (6 female, ages 38-61) on the International Space Station (ISS), most for >6 months. They collected blood <48 hours *before* return to Earth and analyzed quickly upon return./22 

Here’s a figure from their 2017 @BMC_series BMC Hematology paper (now a defunct jounal): astronaut Nicole Stott @Astro_Nicole is doing phlebotomy on herself while up on the #ISS, in preparation for the analysis. In this situation, delays in analysis were less of an issue./23 

Key findings: RBC concentration was significantly *elevated* at all 3 in-flight time points. Hb was elevated early in flight by ~12%, returned to pre-flight levels during the mission, & fell below baseline levels on landing day. There were no variations in MCV or other cells./24 

Our journey into space continues momentarily! Twitter still insists on chunking tweetorial in blocks of 25.) If space travel one day becomes like airline travel, will a layover en route to a final destination be called an “inter-mission”? Most Americans don't care, it seems./25 





The Longitudinal Study of Astronaut Health (LSAH; Trudel et al AJH 2019) recruited 721 mission‐astronauts w/ 3:1 controls: 17,336 hemoglobin measurements. Among these, 92 (12.9%) of astronauts missions reached the WHO definition of anemia on at least 1 post-flight blood draw./26 

The prevalence of anemia in the LSAH cohort was 7% for short duration missions, 10% for medium duration, and 48% for long duration missions. Keep in mind that astronauts returning from missions longer than 120 days have all their circulating erythrocytes produced in space.../27 



...and also that erythropoietin changes take 7 days to alter Hb; that's just how red cell kinetics works. Image: Elliott S et al Ann Hematol 2014/28 

*Thrombosis* is also a concern in space, likely due to altered blood flow induced by microgravity.
Blood flow reversal can even occur. In 2019, an astronaut on the ISS developed an internal jugular thrombosis, probably from sluggish flow +/- microtrauma./29
Blood flow reversal can even occur. In 2019, an astronaut on the ISS developed an internal jugular thrombosis, probably from sluggish flow +/- microtrauma./29
Enoxaparin in the ISS medical kit (!) was started and “multispecialty discussions ensued.” Apixaban was flown up to the space station (!) VTE expert Stephen Moll @UNC_Health_Care, who is a character, gave critical advice & offered to go up to the ISS for in-person consult.😀/30 



@NASA and various academics have carefully studied Mark and Scott Kelly, identical twins who are both astronauts and who therefore provide a unique chance to analyze environmental effects without confounding by germline variation./31 

Changes with space exposure were observed in telomere length, gene regulation (measured by both epigenetic and transcriptional data), gut microbiome, body weight, carotid artery dimensions, subfoveal choroidal thickness and total retinal thickness, and serum metabolites./32 

“In addition, some factors were significantly affected by the stress of returning to Earth, including inflammation cytokines and immune response gene networks, as well as cognitive performance.” Vaccine response seemed unaffected by space travel. /33
For a few measures, persistent changes were observed even after 6 months back on Earth, including gene expression levels (hard to know what that means), increased chromosome alterations and short telomeres. This may have implications for long missions, such as to Mars./34 

Chromosome changes had been observed in blood cells of returning astronauts previously. Which begs the question: /35 

Ham (the famous chimpanzee from Cameroon who went to space on Mercury 2 in 1961, shortly before John Glenn) was the first “space chimp”. In his honor, shouldn't we call this phenomenon “Space CHIP” – i.e., clonal hematopoiesis of indeteminate potential induced by space flight?/36 

@StationCDRKelly's memoir “Endurance: A Year in Space, A Lifetime of Discovery” about his childhood, Navy ROTC & Naval test pilot experience, and NASA career (including a >1 year ISS mission) is well worth reading. I got it shortly after it came out and enjoyed it./37 



Finally–there has been a hiatus in #HematologyTweetstories of late, as @dgkhalaf keeps reminding me.🙂 That reflects moving to a new job in December & learning new social media policies, moving house, and also recovering from COVID, which was exhausting & made December a hash./38
But I promise I will continue to create a #HematologyTweetstory now and again, as long as people seem to be interested - so far so good! I hope you enjoyed this short hematological journey outside of the terrestrial bounds.🌎🚀🛰️ /39End
• • •
Missing some Tweet in this thread? You can try to
force a refresh