1/ At a recent @MEActNet briefing, Dr. Anthony Komaroff confirmed his earlier prediction that we had reason to expect some w/ COVID-19 would develop a debilitating chronic fatigue syndrome w/ symptoms similar to post-viral #MECFS (focusing on #LongCovid cases w/o organ damage). 
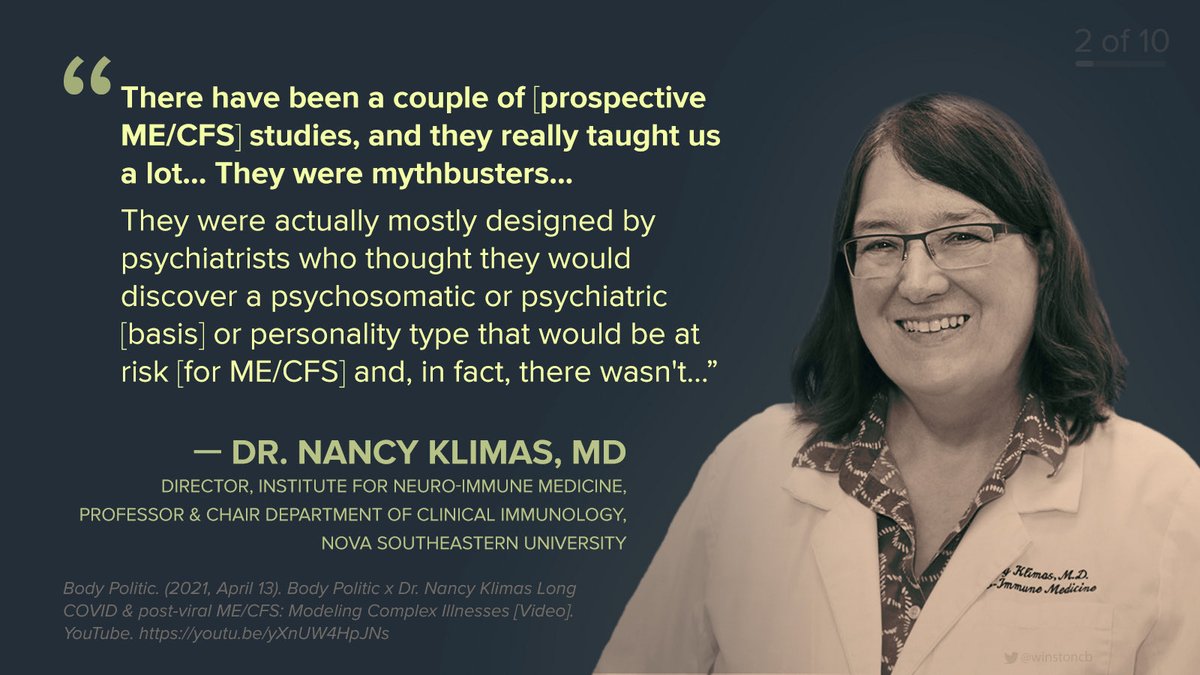
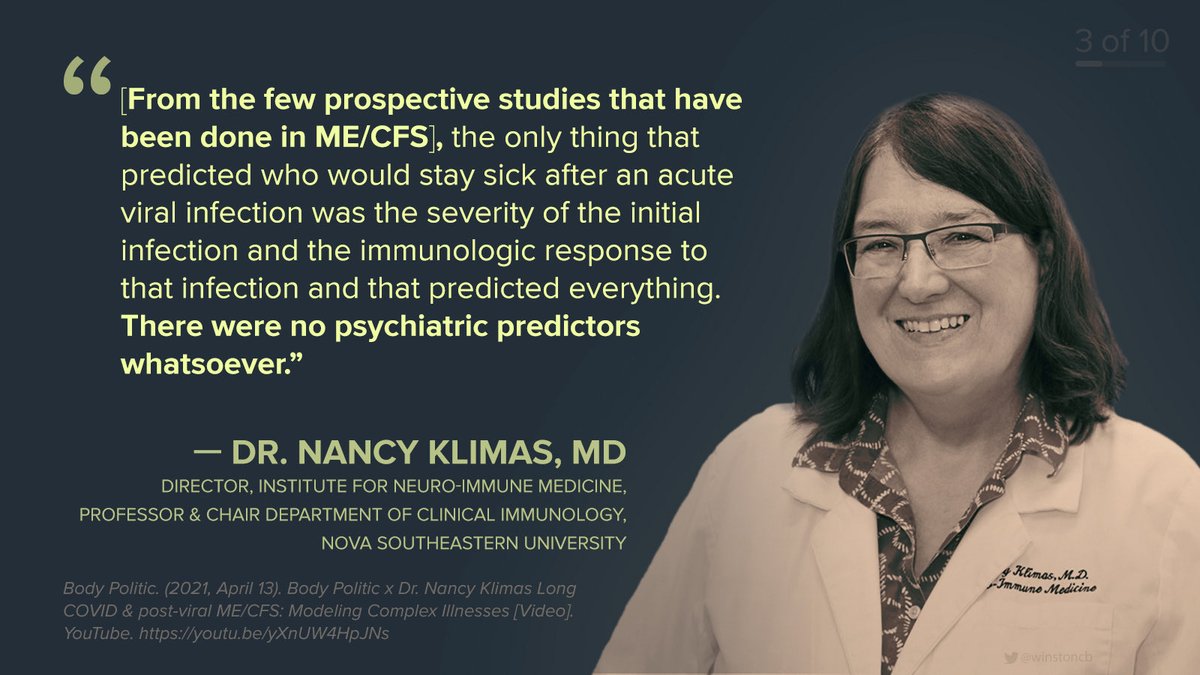
2/ Komaroff alluded to abnormalities found in the brain in #MECFS, referencing theory of chronic low-grade activation of immune system in the brain — requires validation. Called for #LongCovid studies to build off past ME/CFS findings, plus research including both patient groups. 
3/ Komaroff proposes that #MECFS is an illness “with a final common pathway that can be triggered by different things". 
4/ As such, #LongCovid and #MECFS triggered by other viruses, infections, or environmental factors, could potentially be treated with similar interventions, even if there are some differences, such as higher incidence of symptoms related to smell, taste, and shortness of breath. 

5/ So how might #LongCovid benefit from decades of research into #MECFS? First of all, “we know there are multiple abnormalities of the brain and the autonomic nervous system [in ME/CFS], which controls vital functions of the body...” 
6/ Second, in #MECFS “we know there is sort of a combination of activation, dysregulation, and exhaustion of different parts of the immune system,” and this may explain symptoms in #LongCovid too. 
7/ Third, in #MECFS we know there are abnormalities of metabolism, particularly energy metabolism, w/ growing evidence that cells are unable to make adequate amounts of ATP. This could explain symptoms like exertion intolerance, fatigue, and weakness also seen in #LongCovid. 
8/ Fourth, a state of chronic oxidative stress has been identified in #MECFS.
And finally, there are signs of abnormalities of the gut microbiome in ME/CFS – involving imbalances in the bacteria and other microbes that may mediate many important bodily processes.
And finally, there are signs of abnormalities of the gut microbiome in ME/CFS – involving imbalances in the bacteria and other microbes that may mediate many important bodily processes.
9/ Most importantly these abnormalities observed in #MECFS likely interact with one another, potentially in a way that exacerbates symptoms and reinforces the state of chronic illness. 
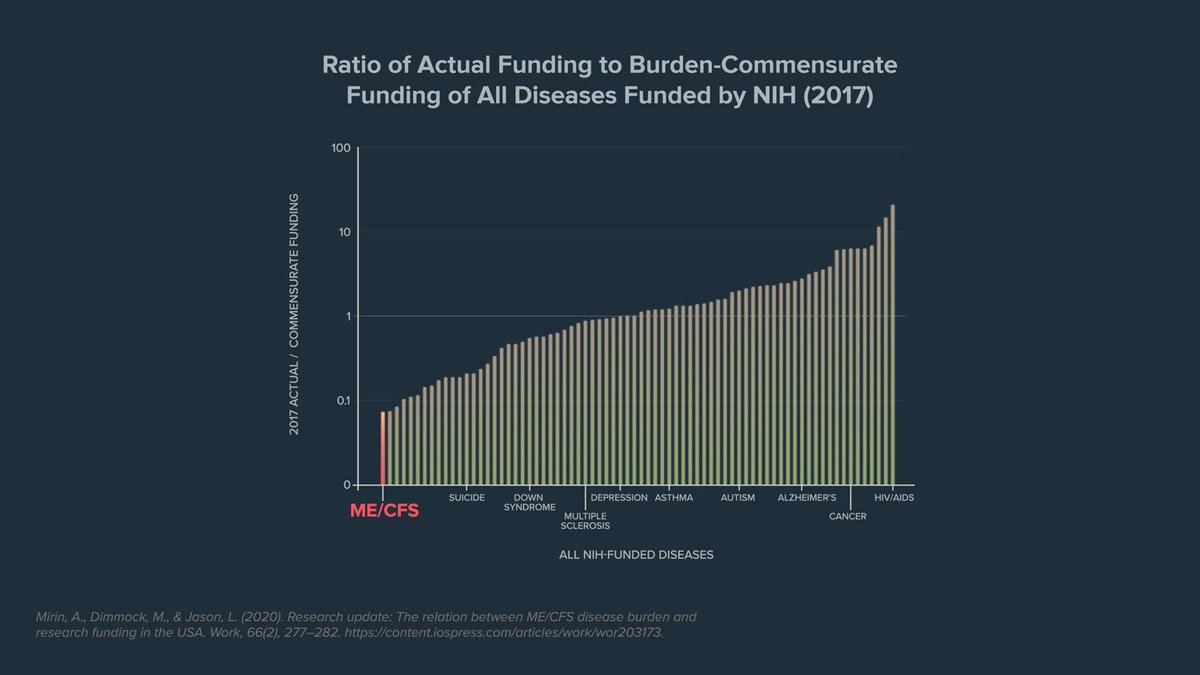
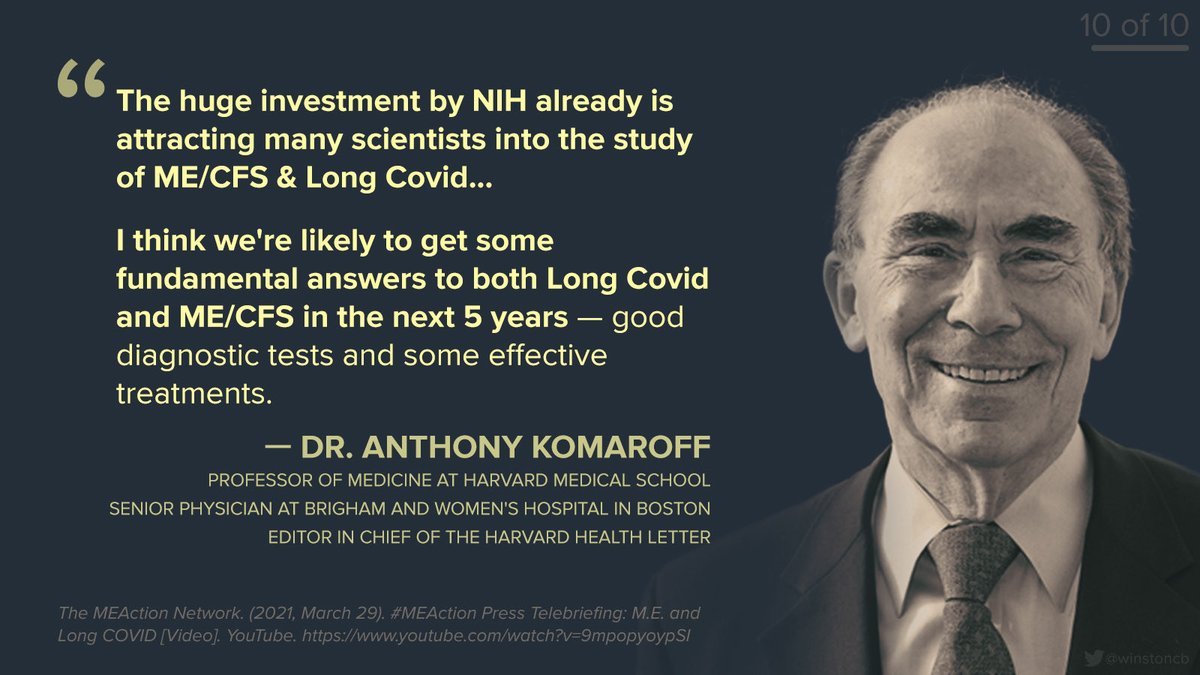
10/ Ever the optimist, Komaroff emphasizes the positive developments and the substantial interest top researchers have shown in studying ME/CFS — not dwelling on the woefully inadequate funding to-date or noting ongoing indifference at the @NIH that continues to impede progress. 
11/ While Komaroff urges that #LongCovid #MECFS be studied together, there are concerning signs the @NIH will continue its neglect of ME/CFS research & patients. i.e. The breakthrough Komaroff predicts will not come for free. 👉 1️⃣solvecfs.org/advoweek21 2️⃣millionsmissing.meaction.net
• • •
Missing some Tweet in this thread? You can try to
force a refresh