1/ Receiving feedback is HARD!
It puts into tension two core human needs:
- To grow🪴 & learn🎓
- To be accepted as we are🫂
Today’s #TweetorialTuesday is going to provide tools to navigate this struggle.
Thanks for joining the @MedEdTwagTeam!
It puts into tension two core human needs:
- To grow🪴 & learn🎓
- To be accepted as we are🫂
Today’s #TweetorialTuesday is going to provide tools to navigate this struggle.
Thanks for joining the @MedEdTwagTeam!
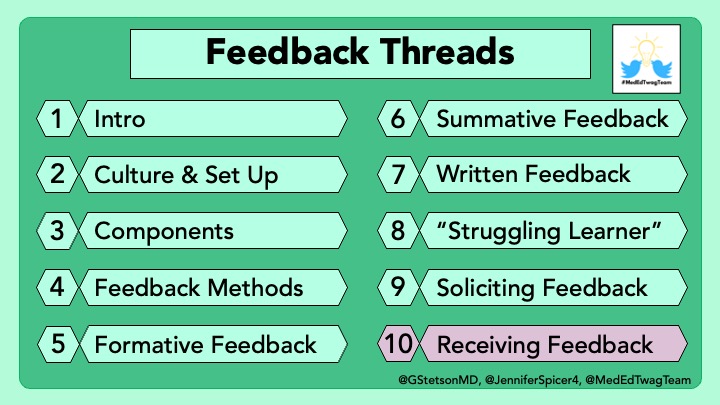
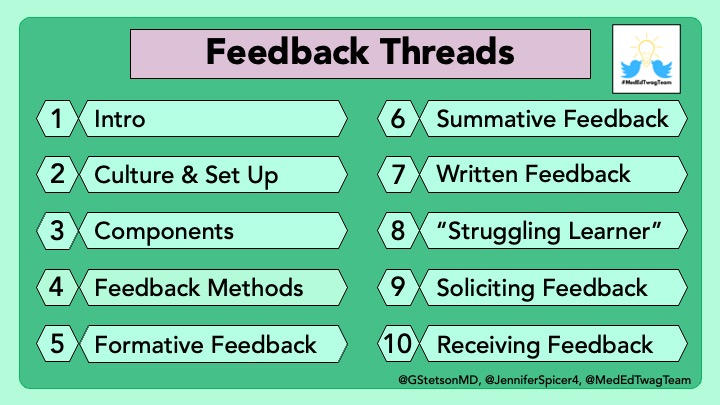
2/ This is our last thread in our #Feedback series (except for a recap next week), and we have saved the best for last.
Many argue that receiving feedback is the MOST IMPORTANT skill.
YOU are the key variable in whether feedback is internalized and applied, not your teachers.
Many argue that receiving feedback is the MOST IMPORTANT skill.
YOU are the key variable in whether feedback is internalized and applied, not your teachers.
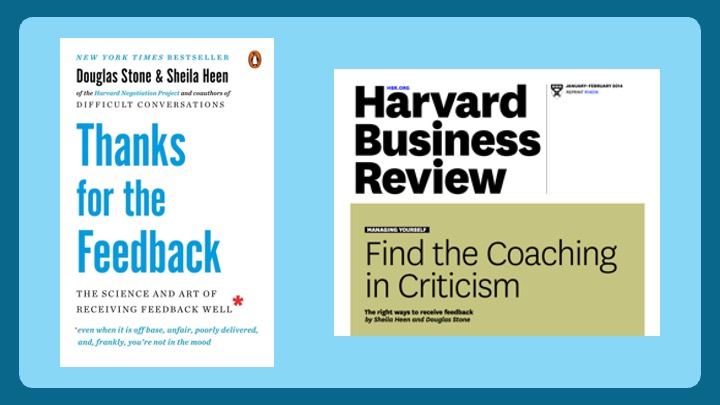
3/ The content of this thread is derived from the work of the feedback gurus, Sheila Heen & Douglas Stone, law professors at Harvard Law School and experts in leadership, collaboration, and conflict management.
Both their book and this paper are definitely worth your time.
Both their book and this paper are definitely worth your time.
4/ Heen and Stone talk about a lot of different things.
I am going to highlight 5 that I feel are most relevant to the clinical learning environment:
I am going to highlight 5 that I feel are most relevant to the clinical learning environment:

5/ 1⃣“Know thyself” – Socrates
Are you generally an optimistic or pessimistic person? Do you react strongly to praise or criticism? Or do you take most things in stride?
If you know your patterns, remind yourself of them so you can be prepared to act how you hope to.
Are you generally an optimistic or pessimistic person? Do you react strongly to praise or criticism? Or do you take most things in stride?
If you know your patterns, remind yourself of them so you can be prepared to act how you hope to.
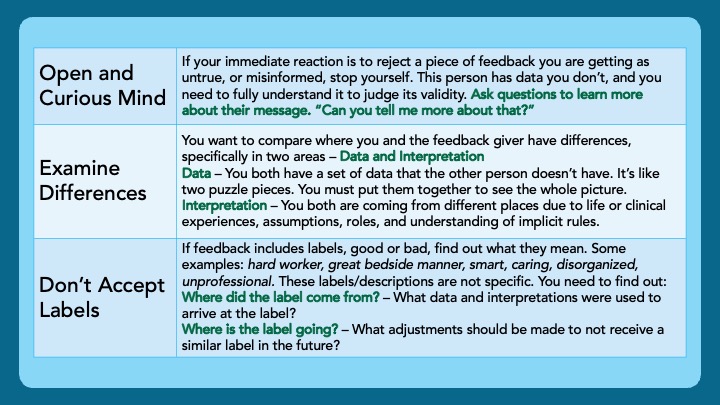
6/ 2⃣Understand the Feedback – Before we determine feedback is valid & something we should incorporate, we first must understand it.
- Enter with a Curious & Open Mind
- Examine Difference – Data & Interpretation
- Don’t Accept Labels – Where did it come from? Where is it going?
- Enter with a Curious & Open Mind
- Examine Difference – Data & Interpretation
- Don’t Accept Labels – Where did it come from? Where is it going?
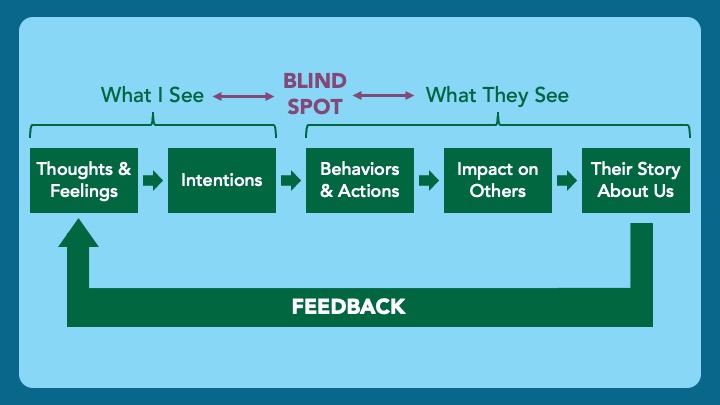
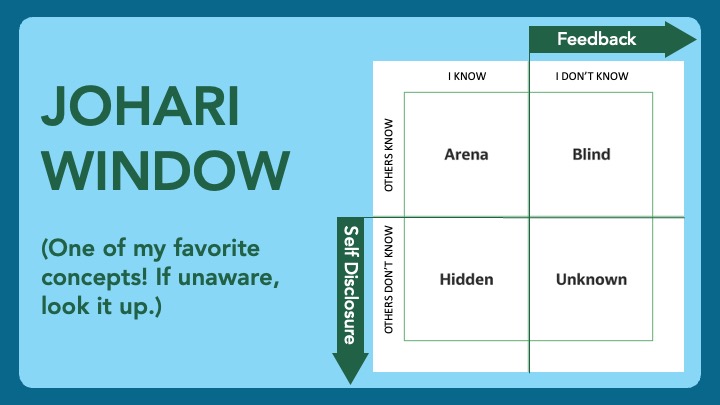
7/ 3⃣See Blind Spots
We judge ourselves on our thoughts/feelings & intentions
Observers judge us on our behaviors, impact on others, & their story about us (their interpretation of our thoughts/feelings & intentions)
Our data is invisible to them. Their data is invisible to us.
We judge ourselves on our thoughts/feelings & intentions
Observers judge us on our behaviors, impact on others, & their story about us (their interpretation of our thoughts/feelings & intentions)
Our data is invisible to them. Their data is invisible to us.
8/ Here is a true story to illustrate difficulties understanding feedback & blind spots.
I was really hurt to get this feedback. But after we heard each others' stories and interpretations, we realized I needed to work on my communication, and not my dedication to patients.
I was really hurt to get this feedback. But after we heard each others' stories and interpretations, we realized I needed to work on my communication, and not my dedication to patients.

9/ Ways to uncover blind spots:
- Observe your reaction
- Look for consistencies
- Get a second opinion
- Record yourself
- Observe your reaction
- Look for consistencies
- Get a second opinion
- Record yourself

10/ 4⃣Control Emotions
Perceived threats to our identity heighten our emotions.
- Practice mindfulness – Observe your body & your breathing. Slow things down.
- Shift to your rational brain – Something we do in medicine all the time. Now apply it to receiving feedback.
Perceived threats to our identity heighten our emotions.
- Practice mindfulness – Observe your body & your breathing. Slow things down.
- Shift to your rational brain – Something we do in medicine all the time. Now apply it to receiving feedback.
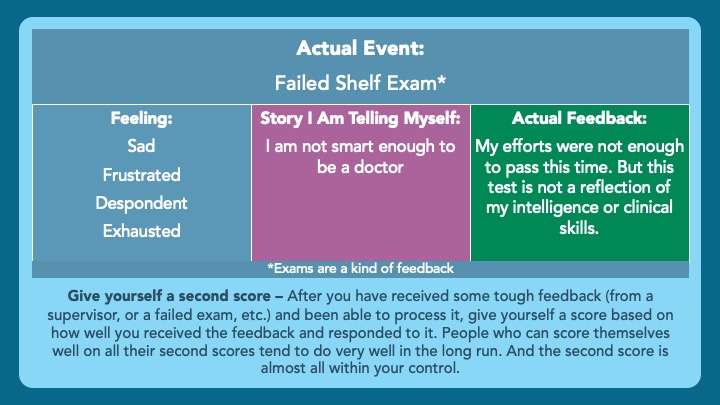
11/ (emotions continued)
- Sort towards coaching – Even if the feedback you are getting is summative/evaluative, put it in the coaching bucket as something that you can use to improve.
- Separate feeling, story, & feedback (see below).
- Give yourself a second score (see below).
- Sort towards coaching – Even if the feedback you are getting is summative/evaluative, put it in the coaching bucket as something that you can use to improve.
- Separate feeling, story, & feedback (see below).
- Give yourself a second score (see below).
12/ 5⃣Be Vulnerable
Our relationships are affected by how we respond to feedback.
When we are vulnerable & share our journey, it allows people to know us better & form stronger connections.
We develop humility, authenticity & confidence.
They feel respected & appreciated.
Our relationships are affected by how we respond to feedback.
When we are vulnerable & share our journey, it allows people to know us better & form stronger connections.
We develop humility, authenticity & confidence.
They feel respected & appreciated.
13/ Again, many argue that how one receives feedback is FAR more important than the way it was delivered.
The five facets of feedback reception I highlighted today were:
The five facets of feedback reception I highlighted today were:

14/ Today was the last #Feedback thread. Thank you so so so much for joining us on this adventure! We loved interacting & learning from you.
Next week, @JenniferSpicer4 will summarize all we have covered. Then, a new topic!
Follow me, Jen, & the @MedEdTwagTeam to not miss out.
Next week, @JenniferSpicer4 will summarize all we have covered. Then, a new topic!
Follow me, Jen, & the @MedEdTwagTeam to not miss out.
• • •
Missing some Tweet in this thread? You can try to
force a refresh