Yesterday’s @WashingtonPost piece on flying-after-vaccination, in which I said I won’t eat on an airplane, created a bit of a kerfuffle. washingtonpost.com/travel/tips/fl… Even @natesilver538 weighed in today.
Let me explain my thinking. (A 🧵) (1/25)
https://twitter.com/NateSilver538/status/1383792830393376774
Let me explain my thinking. (A 🧵) (1/25)
I am fully vaccinated (2 doses of Pfizer in Dec/Jan). As such, I consider myself exceedingly unlikely to get very sick and die from Covid, though as the number of vaccinated people grows, we are beginning to hear about a few breakthrough infections.
cdc.gov/vaccines/covid… (2/25)
cdc.gov/vaccines/covid… (2/25)
Most breakthrough infections are mild but there are rare ones that are serious. Of >75M people fully vaxxed as of 4/13, CDC has logged 5814 breakthrough infctns (documented Covid post-full vaccination). That’s not surprising. As we know, the vaccines aren't 100% protective.(3/25)
Of these 5814, 396 pts (7%) were hospitalized & 74 (1%) died. Of the hospitalized pts, 34% were hospitalized for non-Covid reasons, but as far as we can tell from the report, the rest were Covid-related. It’s vital to put this in context: these are tiny, tiny numbers of… (4/25)
… breakthrough infections, & minuscule numbers of hospitalizations & deaths. If 2/3 of the 74 deaths were also Covid-related, we’re talking 50 deaths from Covid in 75M fully vaccinated people, or a chance of dying from Covid after full vaccination of 1 in 1.5 million.(5/25)
So my mantra that “there is essentially no chance that you will die of Covid after full vaccination” remains correct.
Note that the chance is probably not zero, it's just infinitesimally small. (6/25)
Note that the chance is probably not zero, it's just infinitesimally small. (6/25)
(You may have observed that this risk is similar to the risk of one of these unusual blood clots after the J&J. The essential point is that both of these odds are massively lower than the chances of an unvaccinated person dying of Covid. Please get vaccinated!)(7/25)
Then there's the matter of long Covid. I consider it unlikely that a post-vaccine breakthrough case could lead to long Covid (I have not seen a study addressing this issue) but my guess is that it also can happen, rarely.
So here’s my bottom line, which guides many of... (8/25)
So here’s my bottom line, which guides many of... (8/25)
... my decisions these days: I feel great being vaccinated, I’m doing many things I wouldn’t have done before vaccination, and I no longer worry about getting very sick and dying of Covid.
But – and here’s the key point – I still don’t want to get Covid if I can avoid it.(9/25)
But – and here’s the key point – I still don’t want to get Covid if I can avoid it.(9/25)
This means that I still weigh my risk of being exposed to Covid when I make “safer/not safe?” choices. I completely understand why some people would take a different view: “I’m vaccinated & I don't want to think about risk anymore.” That position will likely work out fine.(10/25)
But for me, while I mostly feel liberated after vaccination, when there’s a somewhat risky situation that I have control over – particularly if it's an activity that isn’t all that important to me – I may make a different choice. Which gets us back to flying & restaurants.(11/25)
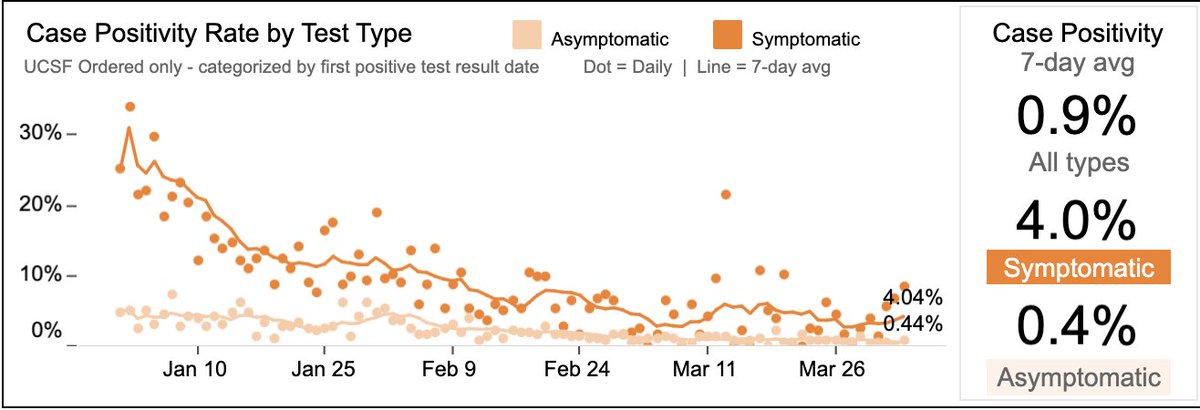
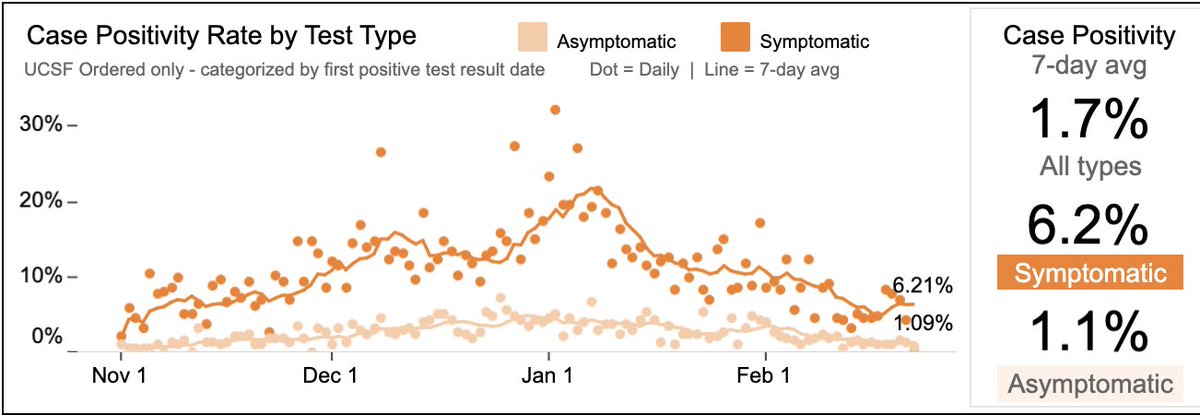
I’m happy to get together in San Francisco in a home w/ vaccinated & even unvaccinated friends/family. Why? The activity is meaningful to me, & SF is a pretty “cool” (Covid-wise) place: test positivity rate 1%, the prevalence of the UK variant is low (West coast variant…(12/25)
…is around, but it doesn’t seem to be as nasty), and there are only a handful of reported cases of variants with potential vaccine resistance.
That said, I still won’t eat indoors at a restaurant yet, though it’s a close call. Why not? (13/25)
That said, I still won’t eat indoors at a restaurant yet, though it’s a close call. Why not? (13/25)
Per CDC, indoor dining has been among highest risk activities. Masks are off most of the time. And, while I know my tablemates, I don’t know the folks at other tables. I like eating in restaurants, but it’s just not that important to me. Ergo: outdoor dining OK, no indoor.(14/25)
Then there's flying. As @washingtonpost piece pointed out, I'm comfortable flying, & have flown 2-3 times in 2021. I won’t take a frivolous trip, but will fly to visit family or for an important work-related event. I consider flying while masked to be exceptionally safe… (15/25)
… for a vaccinated person. And, even for an unvaccinated person, flying while everyone is masked is relatively safe – particularly if neither originating nor destination city (one assumes they're the source of most of the passengers) is particularly “hot”, Covid-wise. (16/25)
But here’s the rub about flying – it is really two different experiences: 1) a 100% masked experience in a clean environment with frequent air exchanges, and 2) an indoor restaurant in the sky.
It's #2 that worries me, even more so than indoor restaurant dining in SF.(17/25)
It's #2 that worries me, even more so than indoor restaurant dining in SF.(17/25)
Why? First, studies have shown that flights are safer w/ middle seats open, but most flights now are packed (they’ve been full on every flight I’ve taken in '21). nytimes.com/2021/04/14/hea… If you fly, you need to assume you’ll be surrounded by strangers at very close range. (18/25)
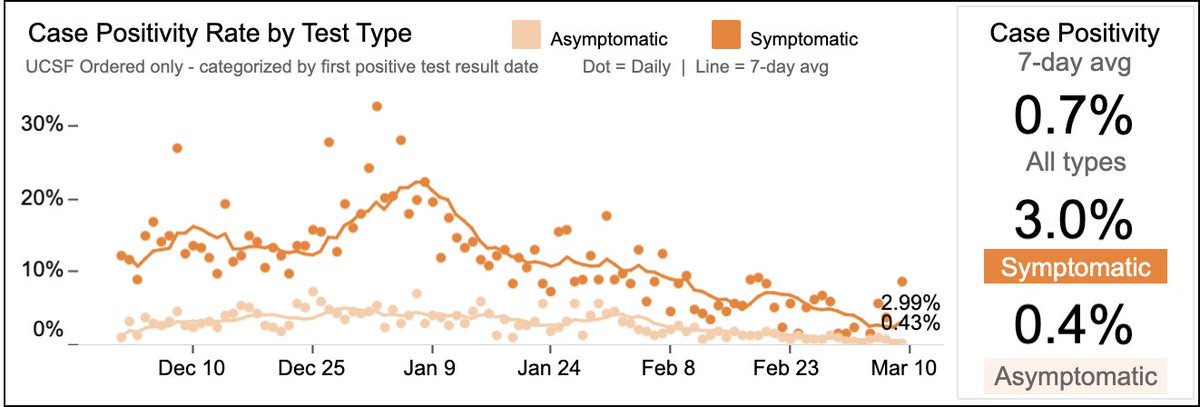
Second, whereas I’m fairly comfortable that a SF restaurant has a Covid likelihood similar to the city's, I’m far less certain about my fellow flyers. Maybe there’s somebody from MI, where test positivity rate isn’t CA’s 1.5%, it’s 16%. Or from Florida, where it’s 10%. (19/25)
And folks may be coming from places where variants are common. I just don’t know. I’m not even sure no one on the plane has a fever or feels sick. (I’d guess that someone feeling ill would cancel a restaurant reservation before they'd cancel a planned flight). (20/25)
Finally, maybe most importantly, I don’t NEED to eat on a plane. And I certainly don’t need to eat while others eat. So my practice on short flights is not to eat at all, taking off my mask briefly (<1 min) at least 30 minutes after meal service to chug a bottle of water. (21/25)
On a longer (eg x-country) flight, I’ll also wait 30 minutes after everybody's done & then quickly eat something. I’ll keep my mask off for the least amount of time necessary.
Neither of these choices seem like that big a deal, and they certainly cause me no hardship.(22/25)
Neither of these choices seem like that big a deal, and they certainly cause me no hardship.(22/25)
Having received Pfizer, I know that the chances of getting infected on a plane are at least 90% lower than the baseline rate, which is ~1/5000 (for unvaccinated people). medrxiv.org/content/10.110…
I’m not at all dogmatic on this; I can understand why someone would make… (23/25)
I’m not at all dogmatic on this; I can understand why someone would make… (23/25)
… a different choice – either because they really love airline food (that's a joke), or, more likely, because they like the feeling of acting “normally” and are sick of playing the 3-dimensional Covid Risk chess game. If that's how someone feels, they should go for it. (24/25)
As for me, while you'll see me on the plane, I'll be the guy with his mask on during meal service. It just makes sense to me. (25/25; end)
• • •
Missing some Tweet in this thread? You can try to
force a refresh