1/ Our paper in @ScienceMagazine asking for "A paradigm shift to combat indoor respiratory infection" was just published
science.sciencemag.org/content/372/65…
science.sciencemag.org/content/372/65…
2/ "There is great disparity in the way we think about and address different sources of environmental infection. Governments have for decades promulgated a large amount of legislation and invested heavily in food safety, sanitation, and drinking water for public health purposes"
3/ "By contrast, airborne pathogens and respiratory infections, whether seasonal influenza or COVID-19, are addressed fairly weakly, if at all, in terms of regulations, standards, and building design and operation, pertaining to the air we breathe."
4/ "We suggest that the rapid growth in our understanding of the mechanisms behind respiratory infection transmission should drive a paradigm shift in how we view and address the transmission of respiratory infections to protect against unnecessary suffering and economic losses."
5/ "It starts with a recognition that preventing respiratory infection, like reducing waterborne or foodborne disease, is a tractable problem."
That's the core of the message: we can reduce respiratory infections a lot, but **we have to try**. So far not tried, except hospitals
That's the core of the message: we can reduce respiratory infections a lot, but **we have to try**. So far not tried, except hospitals
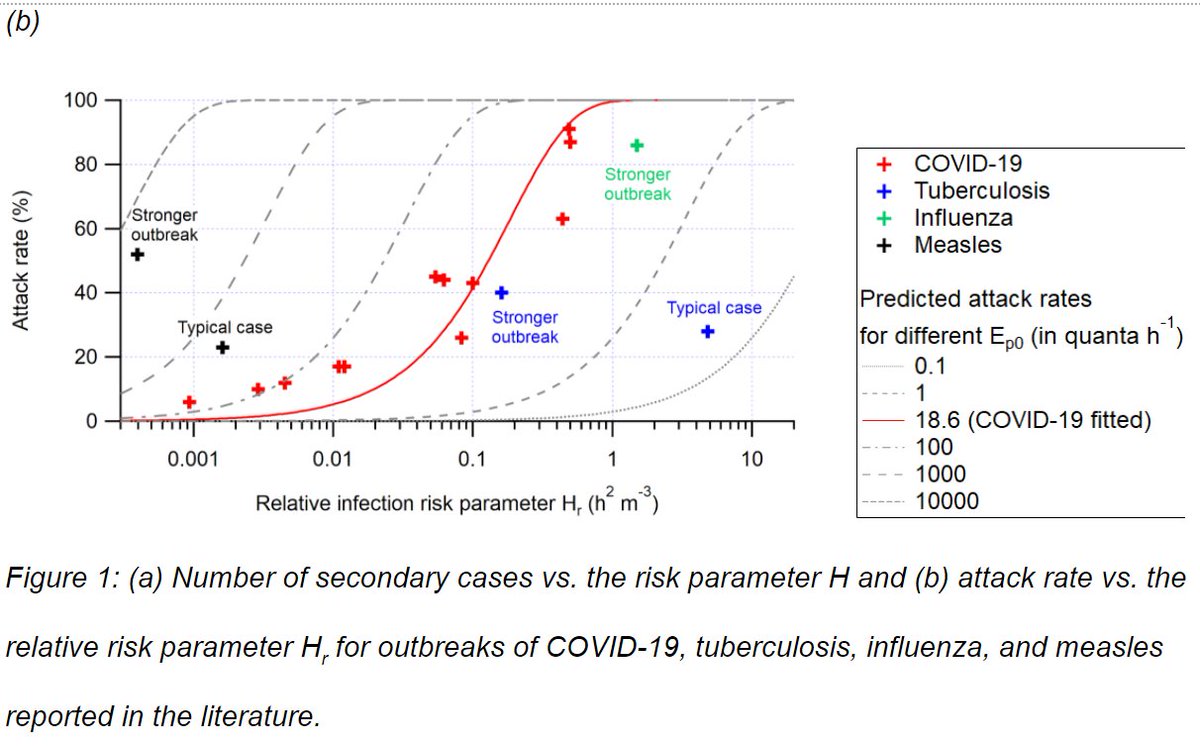
6/ This schematic gives some ideas. Lots of techniques exist that can greatly improve indoor air quality, while balancing energy consumption (which we need to minimize due to climate change, as long as we keep using fossil fuels for energy). 

7/ But it has to start with accepting that COVID-19 and most respiratory infections have important components of airborne transmission.
Which has been denied since 1910, and only accepted as little as possible when undeniable (a pattern that continues for COVID-19).
Which has been denied since 1910, and only accepted as little as possible when undeniable (a pattern that continues for COVID-19).
8/ I have explained the history of the denial on this thread:
(see also @zeyner's article in @nytimes, in Tweet #4 on that thread)
(see also @zeyner's article in @nytimes, in Tweet #4 on that thread)
https://twitter.com/jljcolorado/status/1391111720526024708
9/ And a really well written article on this history was published also today by @MeganMolteni from @WIRED:
wired.com/story/the-teen…
wired.com/story/the-teen…
10/ If the fact that airborne transmission is dominant for COVID-19 is news to you, see our peer-reviewed publication in @TheLancet where we summarize 10 reasons that support it:
https://twitter.com/jljcolorado/status/1383566908797059078
11/ And see this thread for a likely 11th reason, that was published after our @TheLancet paper:
https://twitter.com/jljcolorado/status/1387554983890067459
12/ From ~1910 to 1962, it was accepted that no natural disease displayed airborne transmission.
William and Mildred Wells tried to prove otherwise, eventually succeeded for tuberculosis in 1962. (M. Wells had died by then, and W. Wells would die shortly afterwards)
William and Mildred Wells tried to prove otherwise, eventually succeeded for tuberculosis in 1962. (M. Wells had died by then, and W. Wells would die shortly afterwards)
13/ I find it especially poignant that Prof. William Wells published a paper in a predecessor journal to @ScienceMagazine in 1945, 76 years before our perspective, where he said very similar things to what we just published!
jstor.org/stable/18316
jstor.org/stable/18316
14/ Wells: "The lag in sanitary ventilation during a period of rapid development of water purification, milk pasteurization, and pure food administration is a public health paradox." Yet it was quite natural for sanitary interest in ventilation to lag with the decline..."
15/ "... of infectious diseases formerly attributed to at- mospheric miasma, since close proximity of persons breathing indoor atmospheres made direct transfer of contagious disease without a vehicle a possibility."
16/ Ane Wells goes on to quote Chapin's 1910 fateful denial of airborne transmission:
"Bacteriology teaches that former ideas in regard to the manner in which diseases may be air-borne are entirely erroneous; that most diseases are not likely to be dust-borne, and they are..."
"Bacteriology teaches that former ideas in regard to the manner in which diseases may be air-borne are entirely erroneous; that most diseases are not likely to be dust-borne, and they are..."
17/ "... spray-borne only for two or three feet, a phenomenon which after all resembles contact infection more than it does aerial infection."
The consequences of that denial have haunted us during the COVID-19 pandemic, and underlie the @WHO and @CDCGov denials and resistance.
The consequences of that denial have haunted us during the COVID-19 pandemic, and underlie the @WHO and @CDCGov denials and resistance.
18/ Lots more details about Chapin, Wells etc. in the history thread and in our history preprint:
papers.ssrn.com/sol3/papers.cf…
https://twitter.com/jljcolorado/status/1391111720526024708
papers.ssrn.com/sol3/papers.cf…
19/ The @ScienceMagazine paper was led by Lidia Morawska, collaborating with the "group of 36" scientists that confronted @WHO with the evidence on airborne transmission on 3-Apr-2020 (encountering serious denial), and have worked together since on many papers.
20/ Including @linseymarr @CathNoakes @WBahnfleth @Atze_Boerstra @WargockiPawel @xqcgeo @ShellyMBoulder @Don_Milton Yuguo Li, Raymond Tellier, Julian Tang, Bill Nazaroff, Guy Marks, and many others not on Twitter.
And joined by @trishgreenhalgh @kprather88 @j_g_allen
And joined by @trishgreenhalgh @kprather88 @j_g_allen
21/ The full text of the Science paper has been posted by someone at this link, so you can read it here if you don't have access to Science:
drive.google.com/file/d/1_aMgbc…
drive.google.com/file/d/1_aMgbc…
22/ And this is a press release from @CUBoulder on the paper:
scienmag.com/to-prevent-nex…
Work by @kelcsimpkins with quotes from @ShellyMBoulder and myself
scienmag.com/to-prevent-nex…
Work by @kelcsimpkins with quotes from @ShellyMBoulder and myself
23/ A short article in @nytimes by @apoorva_nyc on the paper:
“We expect to have clean water from the taps,” said Lidia Morawska, and clean, safe food in the supermarket. In the same way, we should expect clean air in our buildings and any shared spaces”
nytimes.com/live/2021/05/1…
“We expect to have clean water from the taps,” said Lidia Morawska, and clean, safe food in the supermarket. In the same way, we should expect clean air in our buildings and any shared spaces”
nytimes.com/live/2021/05/1…
24/ A press release from the UK featuring @CathNoakes with a fitting title:
"Ventilation In Buildings: Where Water Sanitation Was In The 1800s"
scienmag.com/ventilation-in…
"Ventilation In Buildings: Where Water Sanitation Was In The 1800s"
scienmag.com/ventilation-in…
25/ And the press release from QUT, Lidia Morawska's home institution:
Prof. Morawska: need to shift perception can't afford cost of control, given globally harm from COVID-19 of $1 trillion and cost of influenza in the US alone ~$11.2 billion annually
qut.edu.au/news?id=176068
Prof. Morawska: need to shift perception can't afford cost of control, given globally harm from COVID-19 of $1 trillion and cost of influenza in the US alone ~$11.2 billion annually
qut.edu.au/news?id=176068
• • •
Missing some Tweet in this thread? You can try to
force a refresh