Starting off the Nuts & Bolts of Pregnancy and Congenital Heart Disease session with a pre-test question... #CardioObstetrics #ACC21 #ACHD
https://twitter.com/FredWuMD/status/1393601868186755072
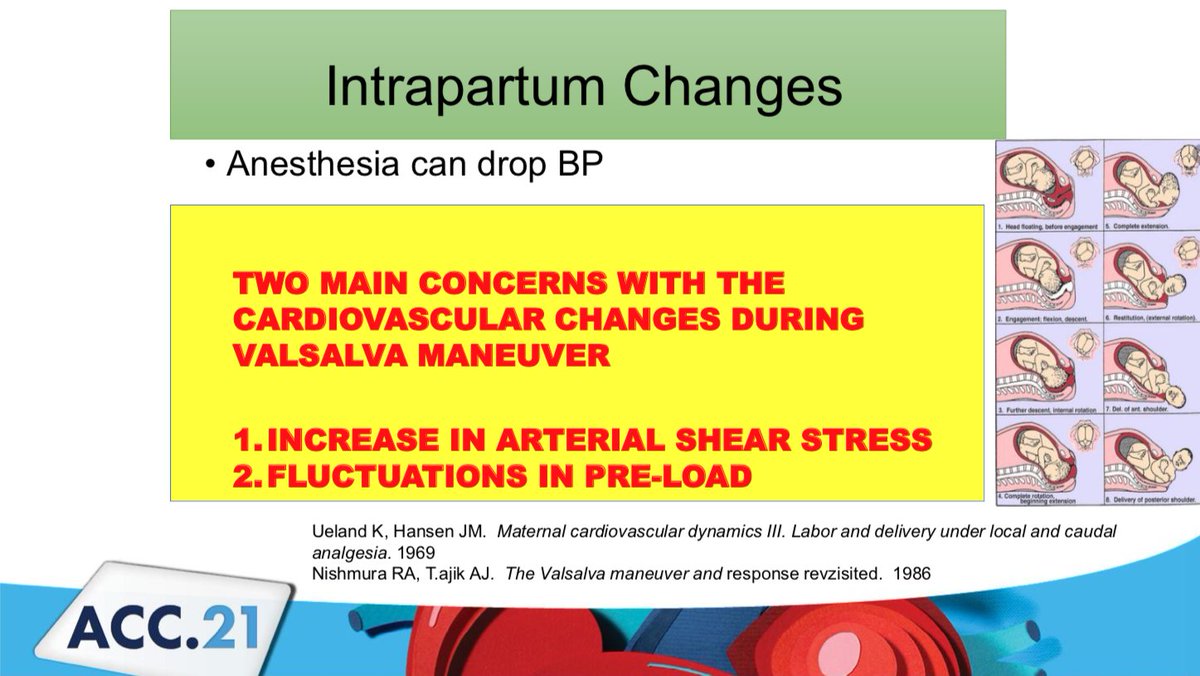
Keep this chart in mind. Pregnancy is a prolonged period of cardiovascular stress with increased cardiac output, plasma volume, and heart rate. Things get really interesting during labor/delivery with acute increases in BP and CO. 

Various risk scores available: Modified WHO classification, CARPREG II, ZAHARA score. But clinical experience is extremely important since CHD patients are very heterogeneous and may not be well-represented in studies 





For preeclampsia prevention, ACOG recommends starting aspirin in high-risk patients. Note: #CHD is *not* considered high risk by this definition, but you don't necessary need to stop ASA for patients who were on it prior to pregnancy. 

Specific L&D concerns for #CHD:
-Contractions result in 300-500mL bolus from uterus to circulation
-BP/afterload can ⬇️ w/anesthesia
-Valsalva drives fluctuations in preload
-After delivery, relief of IVC compression results in autotransfusion, ⬆️ venous return, ⬆️ stroke volume

-Contractions result in 300-500mL bolus from uterus to circulation
-BP/afterload can ⬇️ w/anesthesia
-Valsalva drives fluctuations in preload
-After delivery, relief of IVC compression results in autotransfusion, ⬆️ venous return, ⬆️ stroke volume

Bonus points for a good pun #ACC21 

Two examples of systemic right ventricle: D-TGA with atrial switch, and physiologically corrected TGA. How do we predict CV risk during pregnancy and how do we improve said risk? 

Fundamental differences between anatomic right and anatomic left ventricle:
-Diff. in myofibril arrangement
-Diff. in 3D geometry
-Tricuspid regurgitation (systemic AV valve) very common in systemic RV
-RV supplied by single coronary ? demand ischemia
-Trad HF tx may not apply
-Diff. in myofibril arrangement
-Diff. in 3D geometry
-Tricuspid regurgitation (systemic AV valve) very common in systemic RV
-RV supplied by single coronary ? demand ischemia
-Trad HF tx may not apply

Most recent outcomes data on systemic RV in pregnancy (from @OktayTutarel_MD): No maternal mortality. 10% developed HF, 7% developed arrhythmia. Predictors: pre-pregnancy heart failure, RVEF <40% (Study mostly atrial switch, which is no longer treatment of choice for DTGA) 

Best to optimize systemic RV pt *prior* to pregnancy:
-? intervene on TR
-Consider BB, but AVOID ACE-i, ARB, aldosterone antagonists
-Baseline BNP may be useful
Options to treat HF during pregnancy:
-Diuretics
-Deliver?
-Options for afterload reduction: nitrates/hydralazine
-? intervene on TR
-Consider BB, but AVOID ACE-i, ARB, aldosterone antagonists
-Baseline BNP may be useful
Options to treat HF during pregnancy:
-Diuretics
-Deliver?
-Options for afterload reduction: nitrates/hydralazine

Arrhythmias in Pregnancy:
Increasing freq of arrhythmia in pregnancy, partly due to increased maternal age, partly increase in CV risk factors.
Patients at highest risk: CHD (esp. Fontan, TGA, TOF), cardiomyopathy, acquired heart disease, inherited arrhythmia syndromes
Increasing freq of arrhythmia in pregnancy, partly due to increased maternal age, partly increase in CV risk factors.
Patients at highest risk: CHD (esp. Fontan, TGA, TOF), cardiomyopathy, acquired heart disease, inherited arrhythmia syndromes

Unstable arrhythmia during pregnancy should be cardioverted without delay! DCCV is safe to the baby; only a small amount of energy reaches the fetus. There is a theoretical risk of initiative preterm labor.
Most arrhythmias are pregnancy class C, but adenosine, metoprolol/propranolol, digoxin, lidocaine are considered safe. Amiodarone should be avoided. This graphic is from a great review paper in JACC by @dhalpern10 and @AnneValente1 

From @escardio guidelines:
-For pregnant women presenting w/ SVT, try vagal followed by adenosine (unless unstable⚡️)
-If pt w/ WPW don't use CCB or digoxin due to risk of causing Vfib ☠️
-If AF/AFl in pt w/o underlying structural heart disease, think PE!
academic.oup.com/eurheartj/arti…
-For pregnant women presenting w/ SVT, try vagal followed by adenosine (unless unstable⚡️)
-If pt w/ WPW don't use CCB or digoxin due to risk of causing Vfib ☠️
-If AF/AFl in pt w/o underlying structural heart disease, think PE!
academic.oup.com/eurheartj/arti…

For maternal VT:
-If unstable⚡️
-For VT originating from RVOT, beta-blocker preferred; for fascicular VT, verapamil (I always need an EP doc to determine this!)
-Little evidence in inherited arrhythmia syndromes
-If unstable⚡️
-For VT originating from RVOT, beta-blocker preferred; for fascicular VT, verapamil (I always need an EP doc to determine this!)
-Little evidence in inherited arrhythmia syndromes

• • •
Missing some Tweet in this thread? You can try to
force a refresh