🔟 No mention of 2020 could possibly ignore the effects of the global pandemic on research, patient care, and the way we share knowledge. #COVID19 #ACC21 

9⃣ Imaging indices correlate with prognosis.
- Transplant/VAD-free survival correlates with MPI-DTI z-score
- Left atrial strain correlates with PCWP and helps identify graft rejection/failure
#ACC21

- Transplant/VAD-free survival correlates with MPI-DTI z-score
- Left atrial strain correlates with PCWP and helps identify graft rejection/failure
#ACC21


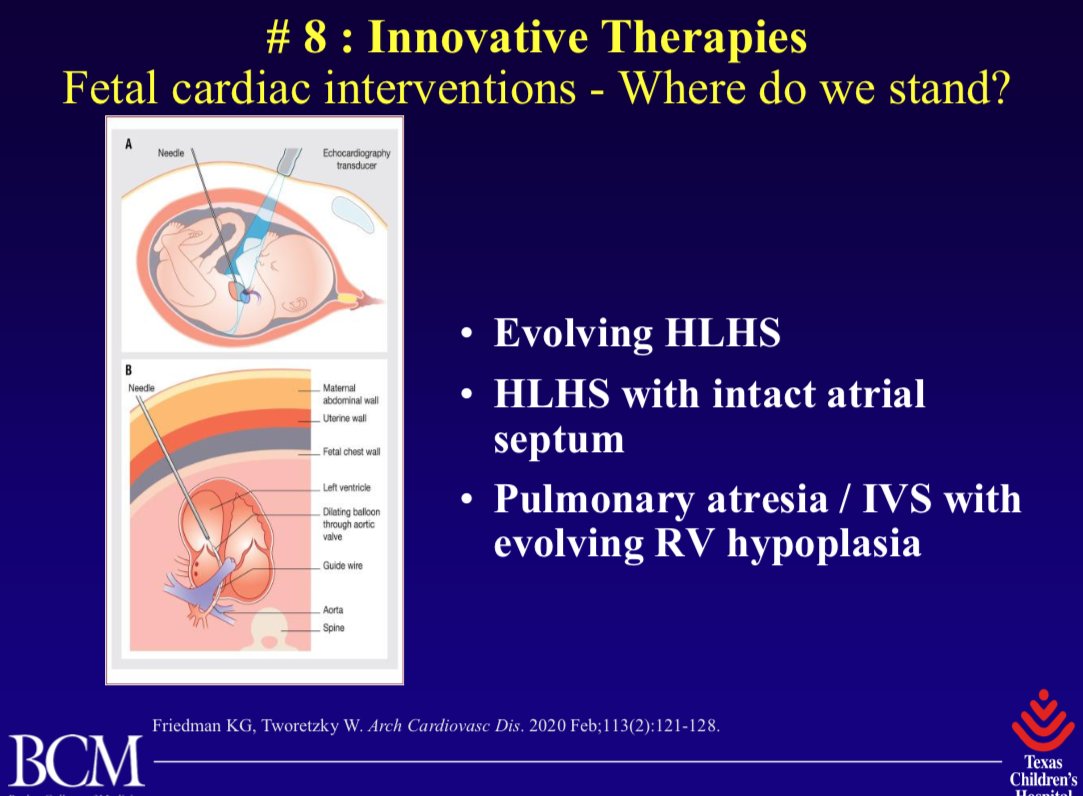
8⃣New concepts in intervention
- Fetal cardiac interventions
- Encouraging results in the Ozaki repair for aortic valve disease
- Encouraging results in sirolimus for preventing restenosis in PVS
#ACC21


- Fetal cardiac interventions
- Encouraging results in the Ozaki repair for aortic valve disease
- Encouraging results in sirolimus for preventing restenosis in PVS
#ACC21


7⃣EP Advancements
- CRT associated with improved transplant-free survival in pediatric and CHD patients
#ACC21
- CRT associated with improved transplant-free survival in pediatric and CHD patients
#ACC21

6⃣Developement of a risk score for interstage death or transplant after stage 1 palliation of single ventricle patients
#ACC21
#ACC21

5⃣Increasing focus on QOL, neurocognitive outcomes, palliative care, and social/racial disparities
#ACC21
#ACC21

2⃣Collaborative research #ACC21 

And finally, a moment to honor two giants in the field of #CHD care who we lost, Dr. Jacqueline Noonan and Dr. William Norwood #RIP
#ACC21
#ACC21

I tweeted the same slide twice, so here are links to the #CHD documents to make it up to you: (1/2)
👉Sachdeva et al. Appropriate Use Criteria for #CHD imaging
jacc.org/doi/full/10.10…
👉Rudd et al. Interstage Home Monitoring for Single Ventricle
ahajournals.org/doi/10.1161/JA…
#ACC21

👉Sachdeva et al. Appropriate Use Criteria for #CHD imaging
jacc.org/doi/full/10.10…
👉Rudd et al. Interstage Home Monitoring for Single Ventricle
ahajournals.org/doi/10.1161/JA…
#ACC21


(2/2)
👉Baumgartner et al. ESC Guidelines for Management of #ACHD
academic.oup.com/eurheartj/arti…
👉Budts et al. ESC Recommendations for Participation in Competitive Sports for Adolescents and Adults with #CHD academic.oup.com/eurheartj/arti…
#ACC21
👉Baumgartner et al. ESC Guidelines for Management of #ACHD
academic.oup.com/eurheartj/arti…
👉Budts et al. ESC Recommendations for Participation in Competitive Sports for Adolescents and Adults with #CHD academic.oup.com/eurheartj/arti…
#ACC21

👉Chowdhury et al. Telehealth for #pedscards
link.springer.com/article/10.100…
👉Foster et al. Telemedicine to enhance in-home interstage care
link.springer.com/article/10.100…
👉Chen et al. Telehealth in pediatric heart transplant patients
linkinghub.elsevier.com/retrieve/pii/S…
#ACC21
link.springer.com/article/10.100…
👉Foster et al. Telemedicine to enhance in-home interstage care
link.springer.com/article/10.100…
👉Chen et al. Telehealth in pediatric heart transplant patients
linkinghub.elsevier.com/retrieve/pii/S…
#ACC21
👉Wright et al. Prognostic significance of tissue Doppler imaging-derived MPI in pediatric pts with DCM
onlinelibrary.wiley.com/doi/abs/10.111…
👉Left atrial strain correlated with elevated filling pressures in pediatric heart transplant recipients
linkinghub.elsevier.com/retrieve/pii/S…
#ACC21
onlinelibrary.wiley.com/doi/abs/10.111…
👉Left atrial strain correlated with elevated filling pressures in pediatric heart transplant recipients
linkinghub.elsevier.com/retrieve/pii/S…
#ACC21
👉Friedman et al. Fetal Cardiac Interventions
sciencedirect.com/science/articl…
👉Marathe et al. Modified Ozaki Procedure in Young Patients
annalsthoracicsurgery.org/article/S0003-…
👉Callahan et al. Systemic Sirolimus to Prevent In-Stent Stenosis in Pediatric PVS
link.springer.com/article/10.100…
#ACC21
sciencedirect.com/science/articl…
👉Marathe et al. Modified Ozaki Procedure in Young Patients
annalsthoracicsurgery.org/article/S0003-…
👉Callahan et al. Systemic Sirolimus to Prevent In-Stent Stenosis in Pediatric PVS
link.springer.com/article/10.100…
#ACC21
👉Chubb et al. Impact of CRT on Transplant–Free Survival in Pediatric and CHD Patients
ahajournals.org/doi/10.1161/CI…
#ACC21
ahajournals.org/doi/10.1161/CI…
#ACC21

👉Ahmed et al. Development of a validated risk score for interstage death or transplant after stage I palliation for single-ventricle heart disease
jtcvs.org/article/S0022-…
#ACC21
jtcvs.org/article/S0022-…
#ACC21
👉Berger et al. New Era of "Exercise Advocacy" Not Restriction
semthorcardiovascsurg.com/article/S1043-…
👉Sood et al. Cardiac Neurodevelopmental Outcome Collaborative
cambridge.org/core/journals/…
👉Steiner et al. Barriers/Facilitators of Palliative Care/Advanced Care Planning
ajconline.org/article/S0002-…
semthorcardiovascsurg.com/article/S1043-…
👉Sood et al. Cardiac Neurodevelopmental Outcome Collaborative
cambridge.org/core/journals/…
👉Steiner et al. Barriers/Facilitators of Palliative Care/Advanced Care Planning
ajconline.org/article/S0002-…
👉Lopez et al. US Mortality Attributable to #CHD From 1999-2017 Exposes Persistent Racial/Ethnic Disparities ahajournals.org/doi/10.1161/CI…
👉Bucholz et al. Socioeconomic Status and Long-term Outcomes in Single Ventricle Heart Disease
pediatrics.aappublications.org/content/146/4/…
#ACC21
👉Bucholz et al. Socioeconomic Status and Long-term Outcomes in Single Ventricle Heart Disease
pediatrics.aappublications.org/content/146/4/…
#ACC21
👉Holzer et al. Registries, Risk Calculators, Risk-Adjusted Outcomes
link.springer.com/article/10.100…
👉Riggs et al. Pediatric heart-lung transplantation contemporary outcomes
onlinelibrary.wiley.com/doi/abs/10.111…
👉OConnor et al. HeartMate 3 in CHD Multicenter Registry Analysis
jhltonline.org/article/S1053-…
link.springer.com/article/10.100…
👉Riggs et al. Pediatric heart-lung transplantation contemporary outcomes
onlinelibrary.wiley.com/doi/abs/10.111…
👉OConnor et al. HeartMate 3 in CHD Multicenter Registry Analysis
jhltonline.org/article/S1053-…
👉Lewis et al. COVID and CHD in NYC
ahajournals.org/doi/10.1161/JA…
👉Barker et al. Considerations for CHD Pts and Echo Providers in COVID
onlinejase.com/article/S0894-…
👉Feldstein et al. MIS-C in the USA
nejm.org/doi/10.1056/NE…
👉Wilson et al. Return to play post-COVID
bjsm.bmj.com/content/54/19/…
ahajournals.org/doi/10.1161/JA…
👉Barker et al. Considerations for CHD Pts and Echo Providers in COVID
onlinejase.com/article/S0894-…
👉Feldstein et al. MIS-C in the USA
nejm.org/doi/10.1056/NE…
👉Wilson et al. Return to play post-COVID
bjsm.bmj.com/content/54/19/…
• • •
Missing some Tweet in this thread? You can try to
force a refresh