Images of Infectious Diseases
42M on obinutuzumab for CLL. 4 mo ago: mild COVID-19 - no specific Rx. 3 mo ago: SARS-CoV-2 mRNA vaccine.
CC: 2 mo on/off fever, cough, dyspnea. NP SARS-CoV-2 PCR neg. Rx as CAP w doxycycline - no response.
CT chest. DDx? Work up? #MayoIDQ next
42M on obinutuzumab for CLL. 4 mo ago: mild COVID-19 - no specific Rx. 3 mo ago: SARS-CoV-2 mRNA vaccine.
CC: 2 mo on/off fever, cough, dyspnea. NP SARS-CoV-2 PCR neg. Rx as CAP w doxycycline - no response.
CT chest. DDx? Work up? #MayoIDQ next

2/
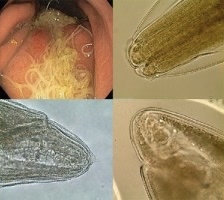
Four months after mild COVID-19, an ICH man with CLL on obinutuzumab presents with prolonged / recurrent doxycycline-non responsive CAP. CT chest shown. See prior tweet for other details. Which of the following is the most likely diagnosis? #MayoIDQ
Four months after mild COVID-19, an ICH man with CLL on obinutuzumab presents with prolonged / recurrent doxycycline-non responsive CAP. CT chest shown. See prior tweet for other details. Which of the following is the most likely diagnosis? #MayoIDQ
3/
All of the MCQ choices could be possible in this case. Imaging suggested viral or PJP.
Work up:
Serum BDG / GM negative
CMV PCR negative
BAL PJP PCR negative
BAL SARS-CoV-2 PCR +++
SARS-CoV-2 spike/nucleocapsid Ab negative (despite infection / vaccine)
All of the MCQ choices could be possible in this case. Imaging suggested viral or PJP.
Work up:
Serum BDG / GM negative
CMV PCR negative
BAL PJP PCR negative
BAL SARS-CoV-2 PCR +++
SARS-CoV-2 spike/nucleocapsid Ab negative (despite infection / vaccine)
4/
Case diagnosis: Persistent COVID-19 pneumonia in B-cell depleted host with CLL Rx with anti-CD20 obinutuzumab
The patient was Rx with IV Remdesivir and high-titer convalescent plasma EUA
Case diagnosis: Persistent COVID-19 pneumonia in B-cell depleted host with CLL Rx with anti-CD20 obinutuzumab
The patient was Rx with IV Remdesivir and high-titer convalescent plasma EUA
5/
Anti-CD20 mAb and infection risk
Pneumonia is most common. “Of the pathogens: 55% bacterial, 12% fungal, including Pneumocystis, Histoplasma, and Aspergillus”
This study did not assess virus causes. Herpes and others have been reported by others.
doi.org/10.1093/cid/ci…
Anti-CD20 mAb and infection risk
Pneumonia is most common. “Of the pathogens: 55% bacterial, 12% fungal, including Pneumocystis, Histoplasma, and Aspergillus”
This study did not assess virus causes. Herpes and others have been reported by others.
doi.org/10.1093/cid/ci…
6/
Anti-CD20 Rx and infection prophylaxis
Obinutuzumab is a monoclonal antibody that targets CD20, which is found on the surface of B cells
Prophylaxis vs. PJP and herpes viruses (HSV / VZV) if anti-CD20 is combined with high dose steroids
Anti-CD20 Rx and infection prophylaxis
Obinutuzumab is a monoclonal antibody that targets CD20, which is found on the surface of B cells
Prophylaxis vs. PJP and herpes viruses (HSV / VZV) if anti-CD20 is combined with high dose steroids
7/
COVID-19 and secondary aspergillus infection
“.....presumed aspergillosis in a cohort of 31 ICU patients...” which may indicate that critically ill COVID-19 patients may be at risk for aspergillosis”
#CAPA covid19 associated pulmonary aspergillosis
doi.org/10.1164/rccm.2…
COVID-19 and secondary aspergillus infection
“.....presumed aspergillosis in a cohort of 31 ICU patients...” which may indicate that critically ill COVID-19 patients may be at risk for aspergillosis”
#CAPA covid19 associated pulmonary aspergillosis
doi.org/10.1164/rccm.2…
8/
Covid-19 and Mucor in India
“The most common causes attributed to the rise of mucormycosis in COVID-19 patients are uncontrolled DM, the use of corticosteroids, and long-term ICU stays.”
doi.org/10.1016/S2213-…
Covid-19 and Mucor in India
“The most common causes attributed to the rise of mucormycosis in COVID-19 patients are uncontrolled DM, the use of corticosteroids, and long-term ICU stays.”
doi.org/10.1016/S2213-…
9/
Persistent COVID-19 in CD20+B cell-depleted hosts
“anti-CD20 Rx adversely impact the development of IgG antibodies and appears associated with delayed clearance of the virus on PCR-based testing”
doi.org/10.1182/blood-…
Persistent COVID-19 in CD20+B cell-depleted hosts
“anti-CD20 Rx adversely impact the development of IgG antibodies and appears associated with delayed clearance of the virus on PCR-based testing”
doi.org/10.1182/blood-…
10/
COVID-19 vaccine responses in CLL Rx with/without anti-CD20
“Ab response to BNT162b2 mRNA vaccine in CLL patients is impaired and affected by disease activity and treatment.”
“No patient on anti-CD20 Rx <12 mo prior to vaccination responded.”
doi.org/10.1182/blood.…
COVID-19 vaccine responses in CLL Rx with/without anti-CD20
“Ab response to BNT162b2 mRNA vaccine in CLL patients is impaired and affected by disease activity and treatment.”
“No patient on anti-CD20 Rx <12 mo prior to vaccination responded.”
doi.org/10.1182/blood.…
11/
Clinical Pearl
ICH patients treated with anti-CD20 may have suboptimal immune response to covid-19 —> leading to persistent infection
Clinical Pearl
ICH patients treated with anti-CD20 may have suboptimal immune response to covid-19 —> leading to persistent infection
/12
Clinical Pearl
ICH patients treated with anti-CD20 may have suboptimal immune response to SARS-CoV-2 vaccine—> may remain at risk of infection (post-vaccine infections have been observed).
Thanks for participating!
Clinical Pearl
ICH patients treated with anti-CD20 may have suboptimal immune response to SARS-CoV-2 vaccine—> may remain at risk of infection (post-vaccine infections have been observed).
Thanks for participating!
• • •
Missing some Tweet in this thread? You can try to
force a refresh