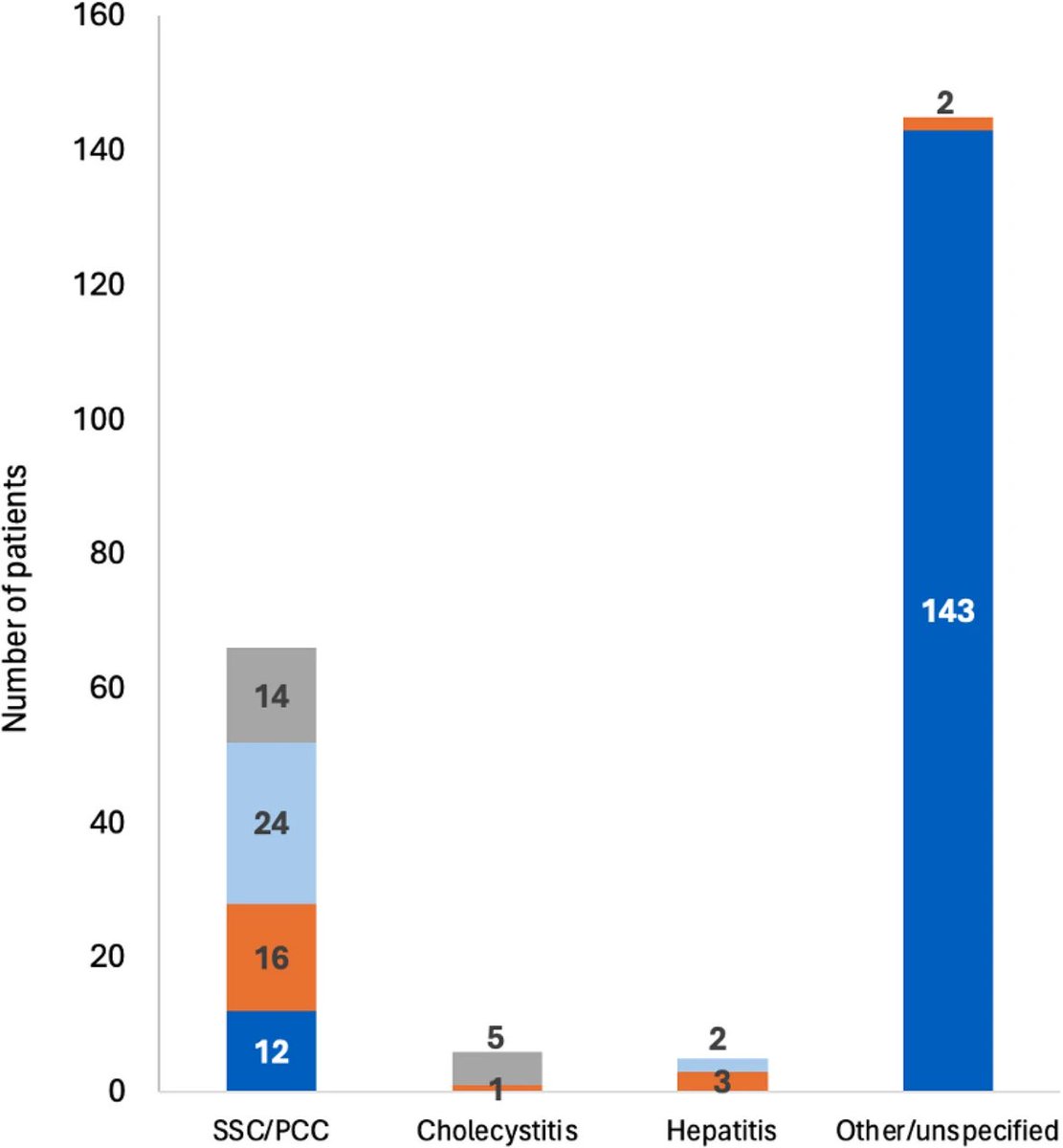
How did #India fare? The graphic tells the whole story:
➡️Brutal onslaught by #B16172: having the highest transmissibility & most immune evader of all VOCs with higher virulence?
➡️No support from Vaccination (negligible coverage & high breakthrough, but reinfections rare) 1/
➡️Brutal onslaught by #B16172: having the highest transmissibility & most immune evader of all VOCs with higher virulence?
➡️No support from Vaccination (negligible coverage & high breakthrough, but reinfections rare) 1/

➡️ Social mitigation measures worked! Or the virus ran out of steam? Or still too early to conclude?
➡️ India struggled (significant mortality/health infrastructure collapsed) but survived!! 2/
➡️ India struggled (significant mortality/health infrastructure collapsed) but survived!! 2/

New study on immune escape potential of #B16172 in comparison to #B1351 w/ #BNT162b2 vaccine: More immune evader than even B1351 VOC! Significant loss of antibody neutralisation vs live B16172 (-5.8x, akin to B.1.351) @TheLancet 3/
thelancet.com/journals/lance…
thelancet.com/journals/lance…

Increased age & time since 2nd dose correlated with reduced virus neutralisation across all strains. Not unusual, but given low starting titres vs #B16172, more of a concern to see neutralisation “dropping off”, significantly. Boosters may be needed!! 4/ 

…………starting from a lower titre (#B16172) means small changes in NAbs titre now likely to have larger effect on vaccine efficacy! 5/ 

More on immune escape with #B16172 & other VOCs by @DavidLVBauer 👇 6/
https://twitter.com/DavidLVBauer/status/1400580669244428289?s=20
• • •
Missing some Tweet in this thread? You can try to
force a refresh