There’s something a bit odd in that CO-CIN data I tweeted on Monday, showing shorter stays in hospital more recently. The problem is, if I use the full dataset to predict the number of inpatients, I get more than there actually were in wave2. 1/n
https://twitter.com/JamesWard73/status/1402026934276702211?s=20
Let’s try that to start with, using a model scenario (I’ll bring in real data in a bit). I’m taking the worst scenario from my recent model update, which has very similar peak hospitalisations to the actual peak in Jan 2021. 2/n
https://twitter.com/JamesWard73/status/1401807703190736897?s=20
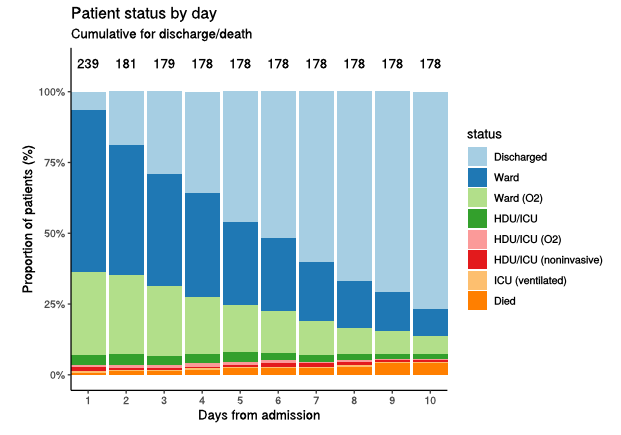
I can run that admissions curve through a simple model which combines it with the CO-CIN data for length of stay, and predicts what the inpatients curve would have been. In fact I get two curves: one using the “recent” data (yellow), and one for the whole dataset (blue): 3/n 

The new data (yellow) produces peak inpatients just shy of 30k, very similar to the peak weekly hospitalisations, and implying an average stay of around 1 week. The older data (blue) has peak inpatients nearly 50k, with a longer average stay. 4/n
The odd thing is that the actual peak inpatients in wave 2 were just under 40k, midway between these two curves. I wondered if the shape of wave 2 was having an impact on this, so I replaced my model scenario with the actual admissions from wave 2: 5/n 

But we get very much the same pattern with the actual data: the recent CO-CIN data gives us the yellow curve, with peak inpatients of ~30k. The full CO-CIN data gives the blue curve, with peak inpatients of ~50k. Neither matches the actual (grey) curve with peak ~40k. 6/n
So what to make of this? I’m not really sure, and welcome insights/suggestions particularly from those with insight into the hospital system. I would expect the full CO-CIN data (blue) to match the actuals (grey) more closely than it does (maybe with some variation). 7/n
It may be that I’m modelling it wrong, but I’ve double-checked and it looks OK. It may be that the CO-CIN data for some reason isn’t representative of the whole system, and is biased to longer stays e.g. if it’s excluding some patients who don’t stay in for very long. 8/n
Or it may be that things happened during the Dec/Jan peak that didn't happen at other times e.g. stronger discharge management - but this doesn't come through very strongly in the shape of the curve. 9/n
In any event, while there is a shorter average stay in the more recent data (yellow), this analysis suggests we should be cautious about assuming there’s a big benefit in reducing peak inpatient load – the reduction may be more like -25% (vs. grey) not -40% (vs. blue). /end
• • •
Missing some Tweet in this thread? You can try to
force a refresh