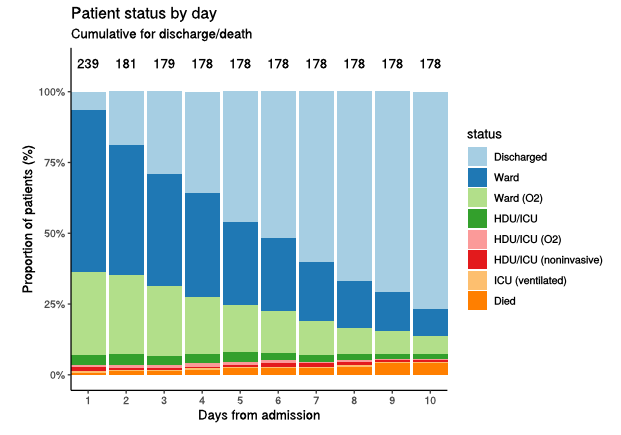
I think this deserves an explanation: why is it that countries that have already completed their epidemics with Alpha (or similar variants) might have an easier time with Delta than the UK, which was still in the process of opening up when Delta hit? 1/n
https://twitter.com/andrew_lilico/status/1404753873118674947?s=20
The answer has all to do with “overshoot”. For most epidemiological concepts there is an @AdamJKucharski thread to go with them, and overshoot is no exception, so I’ll leave you to explore here if you’d like a reminder of how this works: 2/n
https://twitter.com/AdamJKucharski/status/1305436391707467776?s=20
Now for the purposes of this illustration, let’s assume we have two variants:
A, which has R0 of 4.0 and therefore -in a simple model- a herd immunity threshold (HIT) around 75%,
and B, which is 67% more transmissible than A, and so has R0 of 6.7, and HIT of ~85%. 3/n
A, which has R0 of 4.0 and therefore -in a simple model- a herd immunity threshold (HIT) around 75%,
and B, which is 67% more transmissible than A, and so has R0 of 6.7, and HIT of ~85%. 3/n
To start with, variant A is dominant, and after a successful vaccination campaign the city of Bigpharmia (h/t @BristOliver again) has reached a population immunity level of 70%, just shy of the HIT for variant A of 75%. They decide to open up, and incur a small exit wave. 4/n
The size of that exit wave is governed by the distance between their current immunity level, and the HIT. R will be above 1, and hence cases rising, until immunity reaches the HIT, when R will come down to 1. But cases don’t stop there, they keep going – albeit with R<1, 5/n
…and case rates will fall until they become negligible. For relatively small waves that aren’t too near 100% immunity, the wave will tend to be roughly symmetric around the HIT i.e. for every 1% that you start below the HIT, you end up overshooting by about 1% above it. 6/n
So in our example here, Bigpharmia would open up at 70% immunity, and its exit wave would push past the HIT of 75%, coming to rest at around 80% population immunity. I’ve illustrated this in a highly sophisticated hand-drawn picture below: 7/n 

(sorry for short delay, had to go and kill a very large spider in my daughter's bedroom!)
Now let’s suppose variant B takes over. This shifts the HIT up to 85%, and suddenly Bigpharmia is below the threshold again. So (in the absence of intervention), a new exit wave would start. The same rules apply as before, and immunity would run up to around 90%. 8/n 
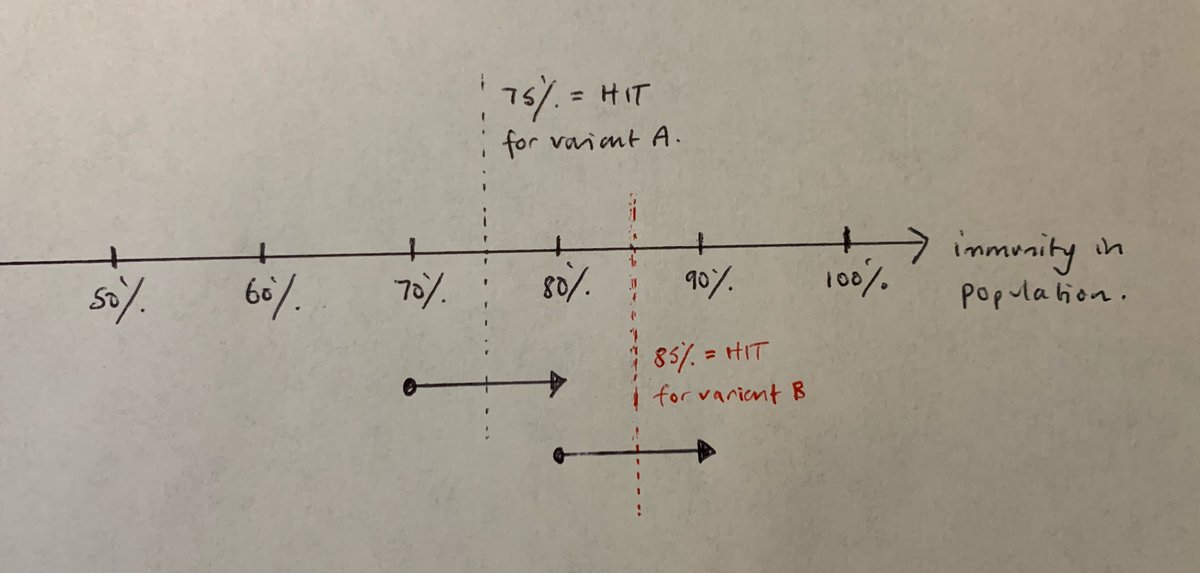
But let’s suppose that Bigpharmia had never had its first exit wave, so it was stuck at 70% immunity when variant B took over. Now it faces the challenge of opening up with 70% immunity, and a 85% HIT. That’s going to create a much bigger exit wave, and if it stayed…. 9/n 

…symmetric around the HIT, it would keep going until pretty much everyone who was still susceptible had caught the virus. (in practice, the dynamics are a bit more complex when you approach 100% immunity, but I’m going to ignore that for simplicity here). 10/n
So we’ve ended up with an extra 10% of the population getting infected, as a result of not having completed the epidemic with the earlier, less transmissible variant A. Put another way, the exit wave for A might infect 10%, but it protects a further 10% from variant B. 11/n
Some have used this logic to argue that, with the great value of hindsight, we should have taken more risks in our opening-up in the UK, and allowed cases (& hence immunity) to grow with the Alpha variant, which might now give us a stronger position for dealing with Delta. 12/n
I’m not completely sure about that; there are complex dynamics in the UK relating to the timing of our vaccination programme, which might mean that earlier opening would still have created worse outcomes (as we’d have been infecting more vulnerable people on average). 13/n
But, whatever your view on that, it’s certainly an argument for why it might be better to “complete” our epidemic with Delta over this summer/early autumn, rather than holding out for a more perfect exit (with fewer deaths and hospitalisations) in the winter. 14/n
One of the risks with holding out is that an even more transmissible variant (or one with greater immunity escape) could appear in the meantime, and we might then be placed in the position that Bigpharmia has above, where we're facing a bigger exit wave than we thought. 15/n
Of course, if we did find ourselves in that position, there are things we could do e.g. by re-imposing moderate controls to flatten the exit wave (or split it into smaller waves), which could reduce the overshoot. But that’s challenging and has costs of its own. /end
• • •
Missing some Tweet in this thread? You can try to
force a refresh