1/
Israel: Missing COVID deaths in the Lancet paper on effectiveness.
NEW information, greater mystery. @federicolois
Israel: Missing COVID deaths in the Lancet paper on effectiveness.
NEW information, greater mystery. @federicolois
https://twitter.com/prof_shahar/status/1404478178676994051
2/
On June 25, the last author of the Lancet paper interviewed on Israeli TV.
She reported that there were 570 COVID deaths of fully vaccinated people in Israel since the vaccination campaign began.
(fully vaccinated = “green pass”= 1 week post 2nd dose)
On June 25, the last author of the Lancet paper interviewed on Israeli TV.
She reported that there were 570 COVID deaths of fully vaccinated people in Israel since the vaccination campaign began.
(fully vaccinated = “green pass”= 1 week post 2nd dose)
3/
Hebrew speakers can read a post by journalist @YaffaRaz including a video clip.
facebook.com/677092628/post…
Hebrew speakers can read a post by journalist @YaffaRaz including a video clip.
facebook.com/677092628/post…
4/
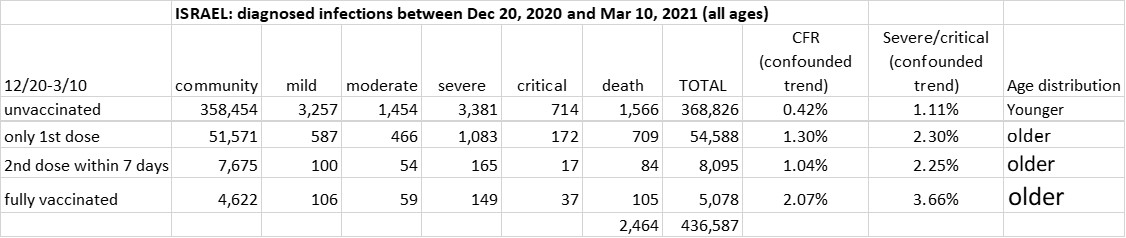
Vaccination campaign started Dec 20.
Longest possible interval for that report on TV: Jan 18 – June 25:
Recall: 570 COVID deaths of fully vaccinated
Lancet paper interval: Jan 24 – Apr 3
Recall: 138 COVID deaths of fully vaccinated (Table).
Difference: 432 deaths
Vaccination campaign started Dec 20.
Longest possible interval for that report on TV: Jan 18 – June 25:
Recall: 570 COVID deaths of fully vaccinated
Lancet paper interval: Jan 24 – Apr 3
Recall: 138 COVID deaths of fully vaccinated (Table).
Difference: 432 deaths

5/
Periods don’t fully overlap, BUT:
~ 1 week at the beginning (not very many fully vaccinated)
Apr 4-June 25, during which there were <200 COVID deaths in Israel (presumably, mostly of unvaccinated)
Who can reconcile the numbers?
Periods don’t fully overlap, BUT:
~ 1 week at the beginning (not very many fully vaccinated)
Apr 4-June 25, during which there were <200 COVID deaths in Israel (presumably, mostly of unvaccinated)
Who can reconcile the numbers?
• • •
Missing some Tweet in this thread? You can try to
force a refresh