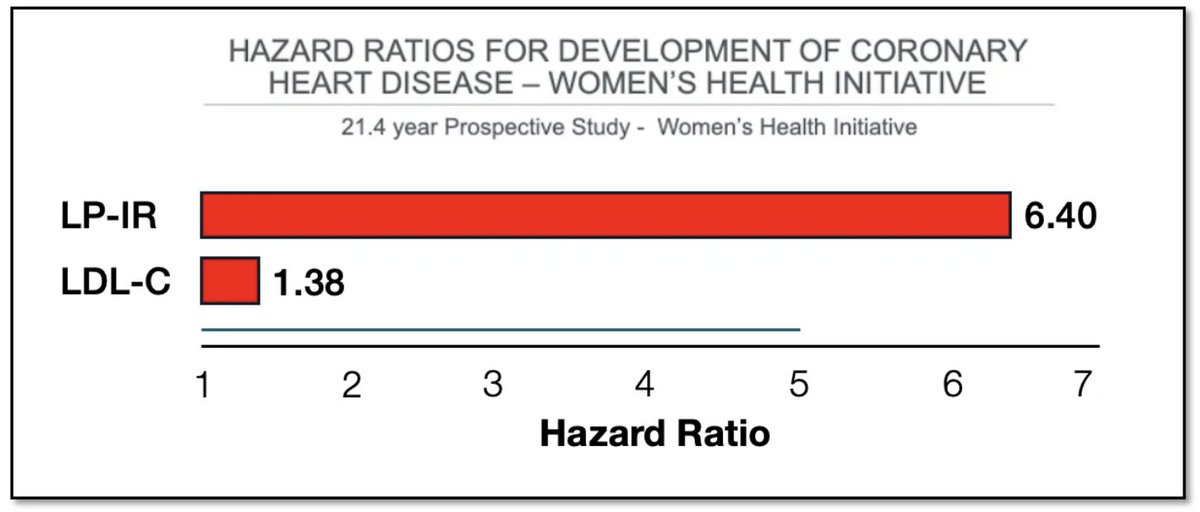
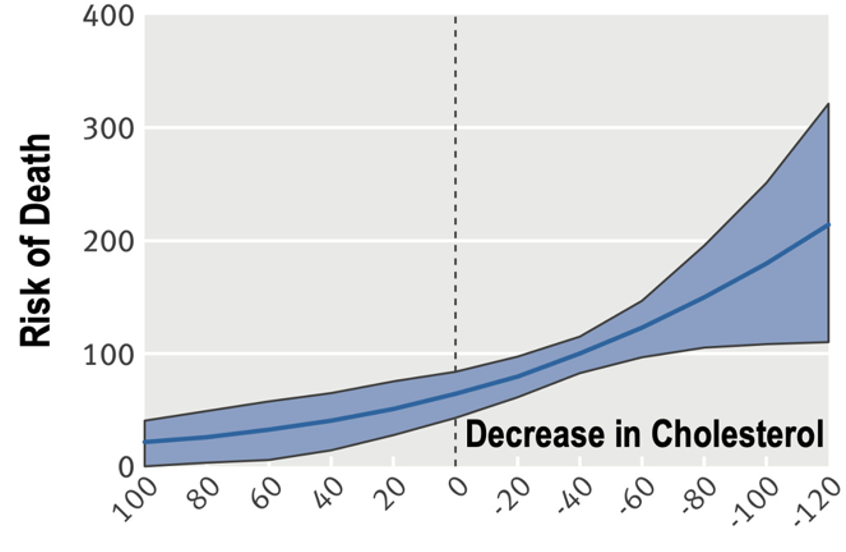
Circulating levels of Lipoprotein Lipase inhibiting factor ANGPTL8 are associated with increased all-cause mortality and CVD risk .@DaveKeto Thoughts?
#metabolism #cvd #LEM
P.S. (ANGPTL8 aka "betatrophin" in the literature)
nature.com/articles/s4159…
cell.com/trends/endocri…
#metabolism #cvd #LEM
P.S. (ANGPTL8 aka "betatrophin" in the literature)
nature.com/articles/s4159…
cell.com/trends/endocri…

2/ Also, it's all very mechanistic, with ANGPTL4 vs. 3/8 being oppositely regualted by feeding and fasting in a tissue specific manner such that fasting decreases fat storage in adopicytes and feeding promotes it.
And, perhaps, unsuprislingly, the lipid metabolism is...
And, perhaps, unsuprislingly, the lipid metabolism is...

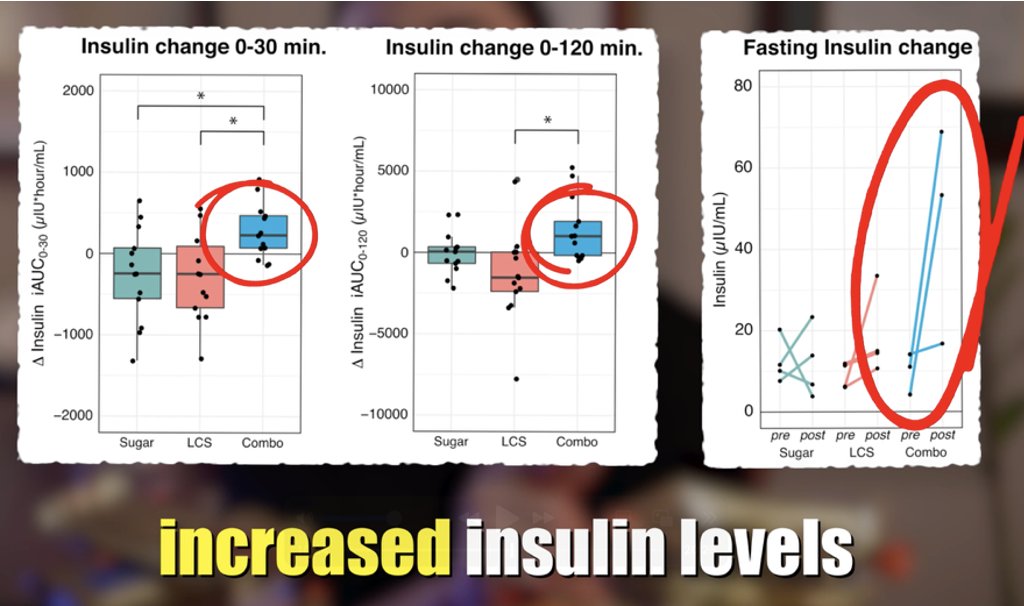
3/ w.r.t ANGPTLs (and specifically 4, which controls local LPL activity) is linked with glucose homeostasis... 


4/ Also, exercise locally induces ANGPTL4 in adipocytes so as to direct fat fuel to working muscles. 

• • •
Missing some Tweet in this thread? You can try to
force a refresh