1/9 Let’s say you are about to do a thyroid exam. Before the exam you do not suspect goiter (pre-test prob of 50%). How does the exam influence your probability? Let’s review some LRs from McGee!
#MedEd #FOAMed #MedTwitter #MedStudentTwitter #EndoTwitter @MedTweetorials
#MedEd #FOAMed #MedTwitter #MedStudentTwitter #EndoTwitter @MedTweetorials

2/9 You may think “well that’s nice, but my thyroid exam technique is not the best.” Don’t worry, the Stanford 25 has got your back (including this clinical pearl)!
stanfordmedicine25.stanford.edu/the25/thyroid.…
stanfordmedicine25.stanford.edu/the25/thyroid.…

3/9 Now that you’ve identified a goiter, you will probably end up ordering some lab and imaging studies. But don’t leave the bedside just yet! Let’s first break down the differential for an enlarged thyroid (thanks again to the Stanford 25). 

4/9 We will need to make sure take a detailed history to prioritize our differential. If you didn’t feel a goiter, make sure to re-examine the thyroid to assess for any nodules. Remember that you can find a thyroid nodule without finding goiter!
5/9 In some cases, the goiter can compress the thoracic inlet when a patient elevates their arm, leading to Pemberton's sign! There is also an image to remind you of the structures that pass through the thoracic inlet. physicaldiagnosispdx.com/cardiology-mul… 



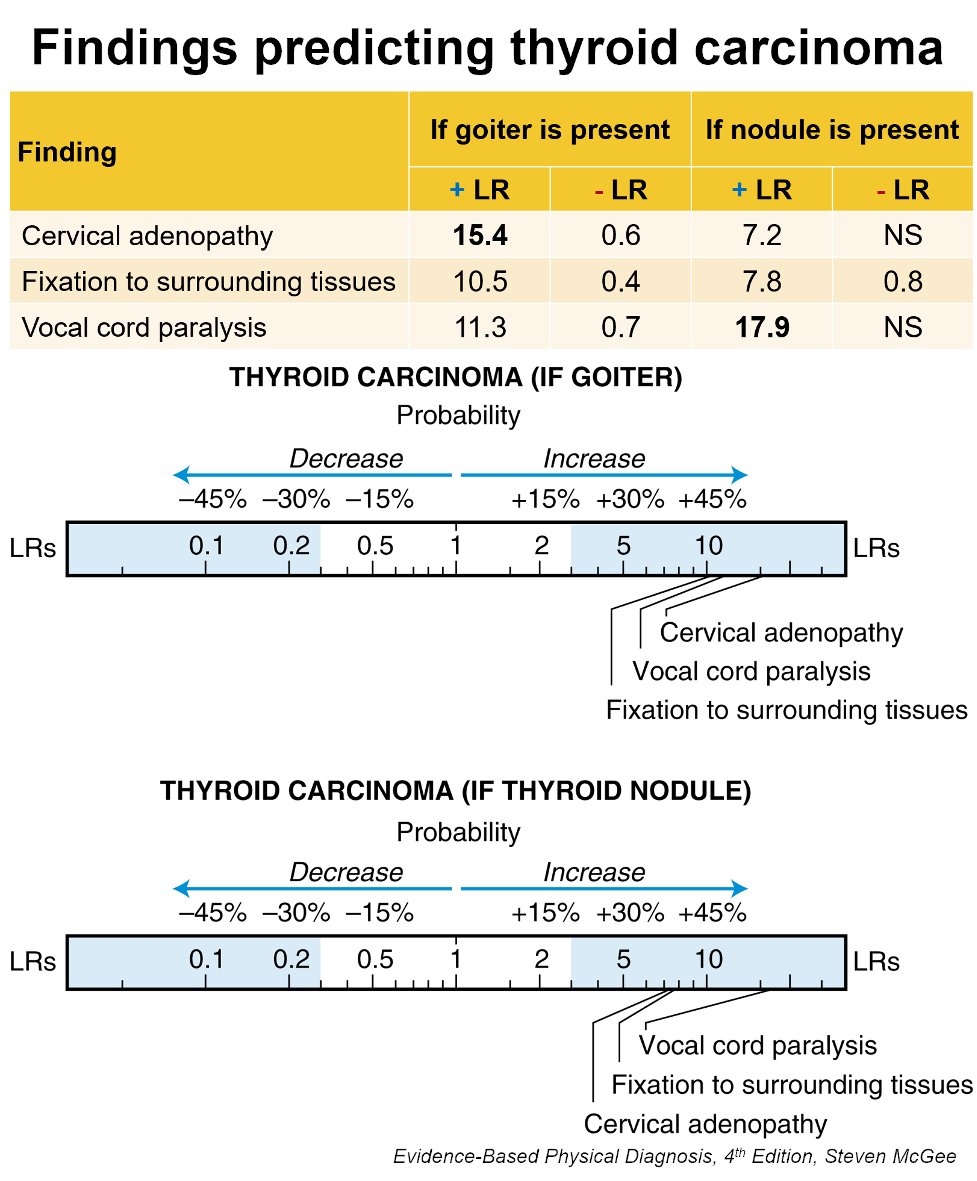
6/9 Let’s focus on 3 exam findings that can help you estimate your post-test probability of thyroid carcinoma (if you find goiter or a thyroid nodule).
1⃣ Cervical adenopathy
2⃣Fixation to surrounding tissues
3⃣Vocal cord paralysis
1⃣ Cervical adenopathy
2⃣Fixation to surrounding tissues
3⃣Vocal cord paralysis
7/9 Here’s a nice guide to assessing 1⃣ cervical adenopathy and a descriptor for 2⃣ fixation (“not freely mobile but rather stuck down to underlying tissue”) meded.ucsd.edu/clinicalmed/he… 

8/9 3⃣ Vocal cord paralysis can be detected based on history of hoarseness, changes in voice, shortness of breath or noisy breathing. Admittedly, these can feel non-specific and diagnosis is ultimately done by otolaryngology.
9/9 Here is a summary using McGee to review how these three findings can influence your probability of predicting thyroid carcinoma (understanding that vocal cord paralysis may be a tough thing to initially diagnose at the bedside). 
• • •
Missing some Tweet in this thread? You can try to
force a refresh









