
Hospitalist @LosAngelesVA | Anesthesiology Intern APD @UCLAAnes @UCLAHealth | Interested in #MedEd, curricular design, and operationalizing stuff | Views my own
3 subscribers
How to get URL link on X (Twitter) App


 2/ Brandon asked the group three questions:
2/ Brandon asked the group three questions:







 2/9 The cornerstone of treatment is to treat the underlying cause. Everything else is just a 🩹. It can sometimes be very hard to treat the underlying cause immediately (assuming you can identify it).
2/9 The cornerstone of treatment is to treat the underlying cause. Everything else is just a 🩹. It can sometimes be very hard to treat the underlying cause immediately (assuming you can identify it). 
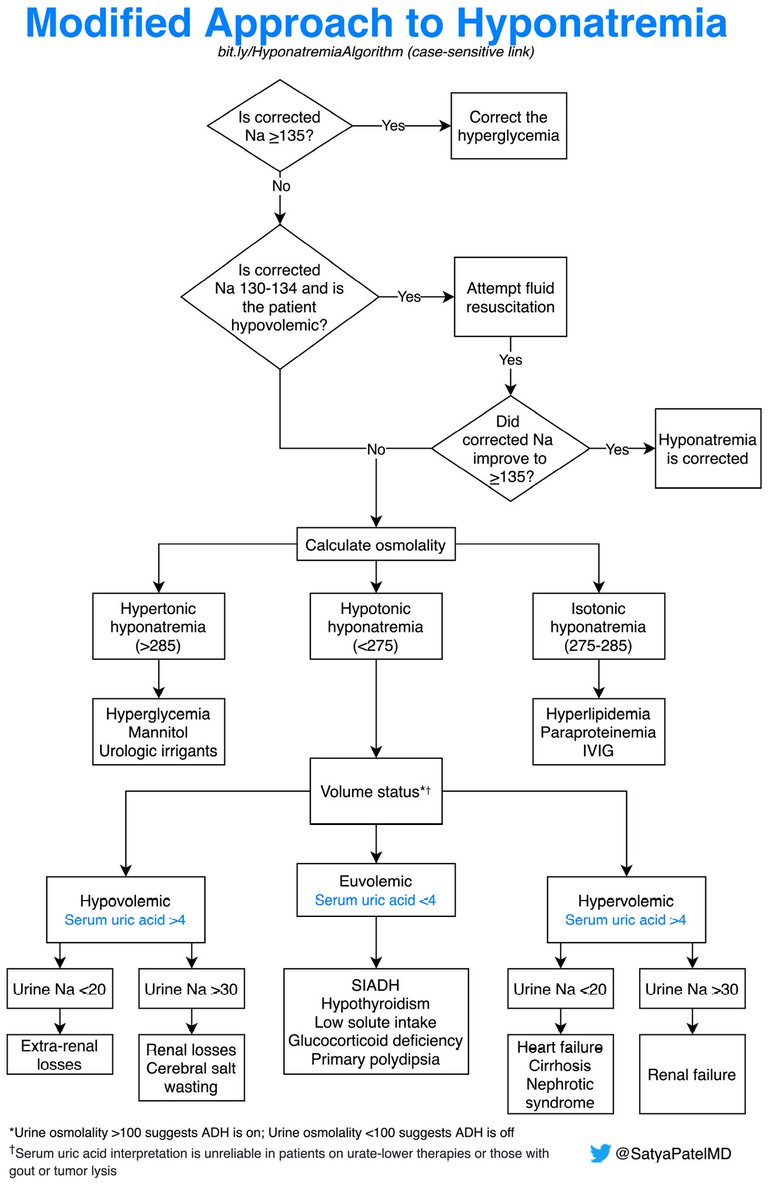
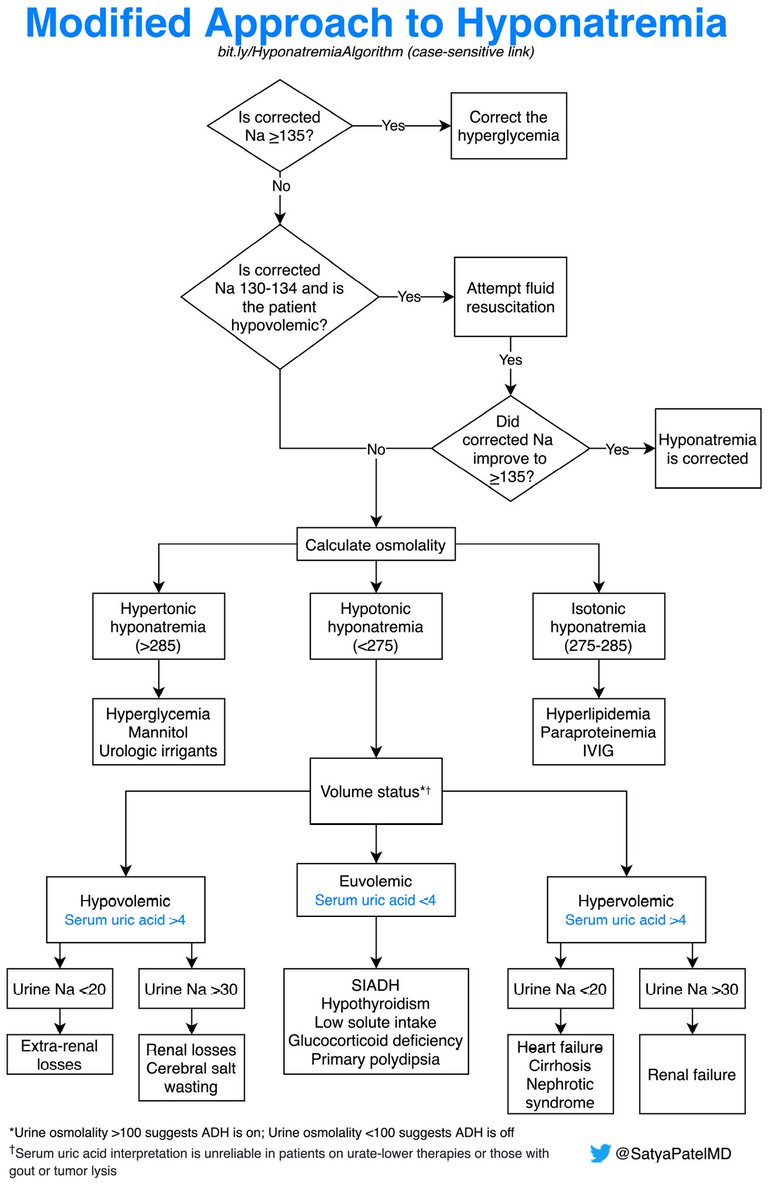
https://twitter.com/SatyaPatelMD/status/1417493742768902144?s=20. Let's keep going.

 2/9 You may think “well that’s nice, but my thyroid exam technique is not the best.” Don’t worry, the Stanford 25 has got your back (including this clinical pearl)!
2/9 You may think “well that’s nice, but my thyroid exam technique is not the best.” Don’t worry, the Stanford 25 has got your back (including this clinical pearl)!




 2/4
2/4 






 2/ What are the Weber and Rinne tests used to help identify?
2/ What are the Weber and Rinne tests used to help identify?
