
When you counsel ICU patients (>65yo)/their proxies before receiving a tracheostomy (‘trach’) and a gastrostomy (‘PEG’), what do you estimate to be the cohort’s 90-day mortality (day 0 = hospital admission)?
When you counsel ICU patients (>65yo)/their proxies before proxies before receiving a tracheostomy (‘trach’) and a gastrostomy (‘PEG’), what do you estimate to be the median number of hospital free days out of 90days in this cohort?
A🧵:When I was a fellow, we had to do rotations through a unit at MGH called the RACU - the Respiratory Acute Care Unit – basically a chronic vent unit after patients got trach/PEGs. @galbamd and @almoskow remember the heartbreak and drama in this unit all too well
The thing I always wondered was: “Is this what patients thought they were getting into???”
(#valueconcordant care)
(#valueconcordant care)
It seemed the biggest factor in whether a pt got trach/peg wasn’t the patient, but whoever the physician happened to be leading the #GOC discussion, in part b/c there wasn’t a lot of objective information to tell the family about what to expect.
Previously we showed that PEG use in ICU pts has dramatically increased over 20 yrs, as ICU survivors increase. Patients with dementia used to be primary users – now ICU pts are #1 utilizer of PEG tubes – about 100,000 ICU pts per year.
https://twitter.com/anicalaw/status/1130445628381814784?s=20
But what happens to all these patients? We used Medicare data to look at patient-centered outcomes after ICU admission. We looked at discharge disposition, mortality, and days-alive-and-out-of-institution (DAOI, aka hospital-free days) in pts who got a trach, PEG, or both.
We found that short-term mortality is very high in pts receiving a trach/PEG/both. Although in-hospital mortality is relatively low (10-17%), most of these patients are sent to SNF/LTCHs, where mortality is very high. Over 40% are dead within 90 days of trach/PEG/both 
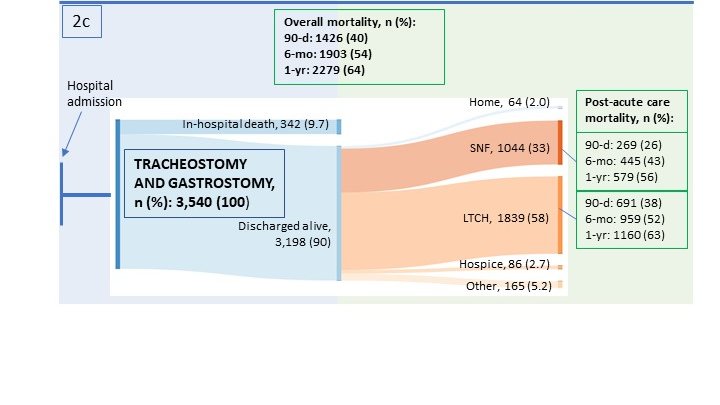
We also found that patients spend very few DAOI after trach/PEG/both. Patients receiving a trach spend a median 3 days out of an institution, while patients receiving a trach and a PEG spend 0 days out of an institution within the first 90 days. 

Some🔑points: we knew 1yr mort in trach patients (and the closely related #PCI/#CCI/#PMV populations) was high (~60%bit.ly/3gqlcgT), but we didn’t know that 90-day mortality was that high. It’s not that “half live a year” – it’s that almost half are dead within 90 days.
In-hospital mortality is NOT a good measurement of short-term mortality because these days (way more than before), most patients leave the hospital before “short-term” is up.
It is very, VERY important to use post-hospitalization data to capture outcomes. Medicare data is one of the few data sources that has linked in-hospital and post-hospital data.
(And yes, data might be better for younger patients – but of note, the majority of our trach/peg patients are >65, so Medicare data made sense).
It’s also time for us to focus on outcomes beyond mortality. We need more #QOL indicators, not just quantity of life. Days alive out of institution (DAOI)/hospital-free days is a start (easy to get from admin databases, integrates mortality/readmission/LOS), and MATTERS to pts
See: pubmed-ncbi-nlm-nih-gov.ezproxy.bu.edu/34319848/ for in-depth discussion on DAOI/HFD @Michael_Harhay @AuriemmaKatie @ScottHalpernMD
A big thank you to @WalkeyAllan @jenintheicu, @rwyeh for their mentorship, and the @SmithBIDMC for their support of this work.
Full paper here! atsjournals.org/doi/pdf/10.151…
• • •
Missing some Tweet in this thread? You can try to
force a refresh



