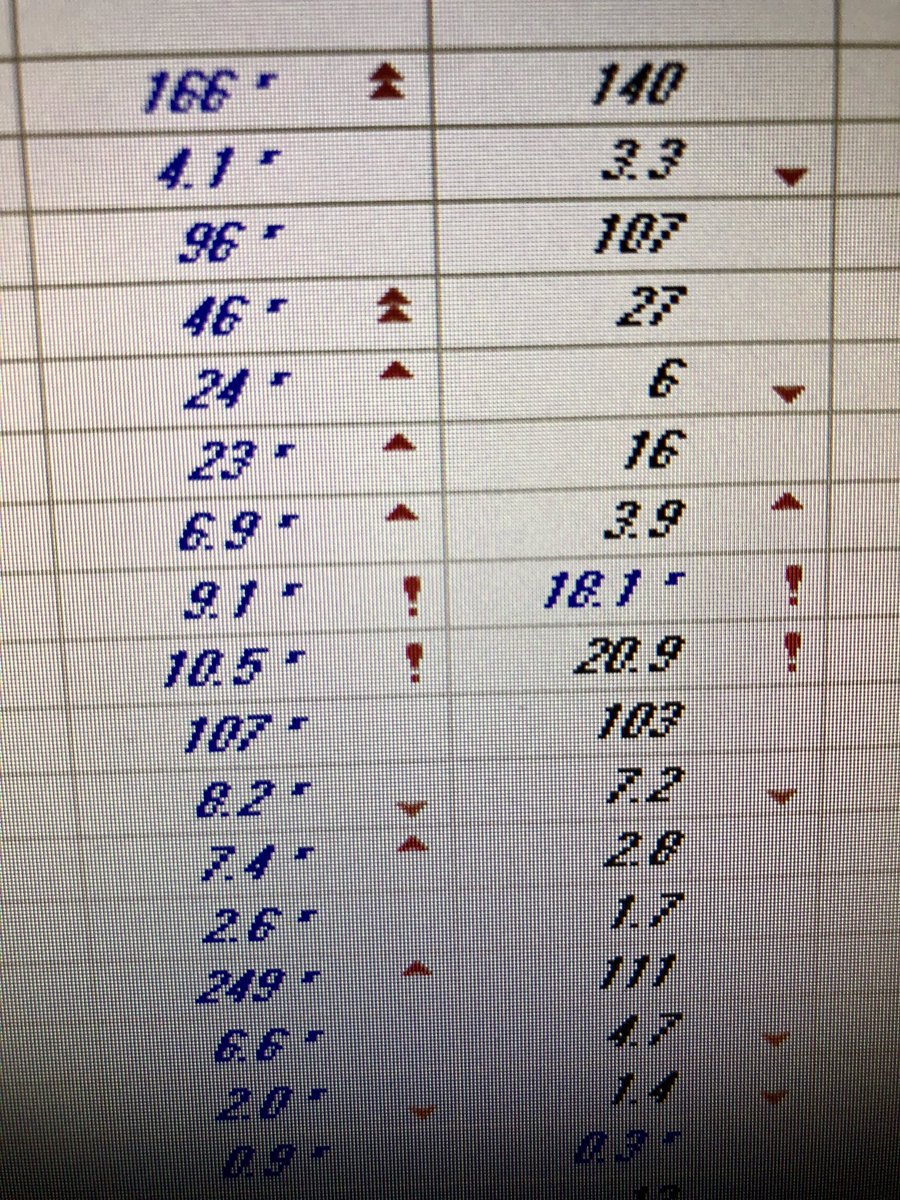
1/x pt w/o polysubstance abuse, MSSA bacteremia 1-month ago, recent heroin/meth use, arrives to ED with 3 weeks of n/v. Vitals normal. Found to be “dry”. BUN/Cr on arrival 135/23 mg/dL. K 7. Anuric, Foley in. Got IVF boluses, shifted. Not better after that, RRT is ordered.
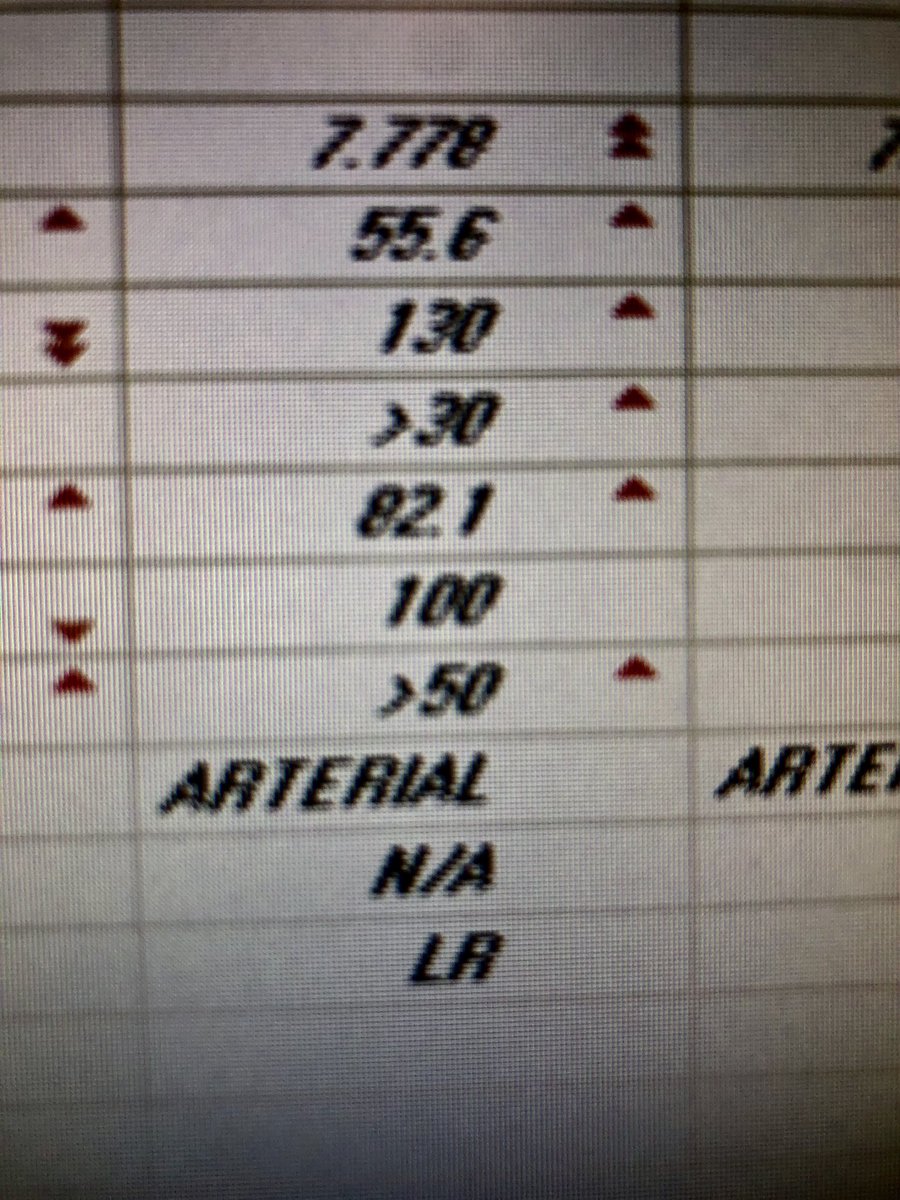
2/x next am post HD, K better. 5-ml urine are obtained and reportedly showed “ATN” urine, granular casts. A renal US is obtained: Left (“baseline” scan, 11.2 cm), right (new scan, 15.2 cm). Report states no hydro, medical renal dz. 

3/x before the US, cognitive bias may lead to conclude early that we were dealing with just a bad ATN, not unreasonable in a pt who vomited and consumed drugs for several days. However, nephromegaly and remarkable ⬆️parenchymal echogenicity seems out of proportion for just an ATN
4/x so, additional 5-ml of urine are obtained. At LPF, there’s a general “ATN” sediment with a few dark casts here and there 

5/x however, at HPF, the truth is revealed: RBC casts are found in fair number (btw, lab later reported hyaline/granular) #UrinarySediment 


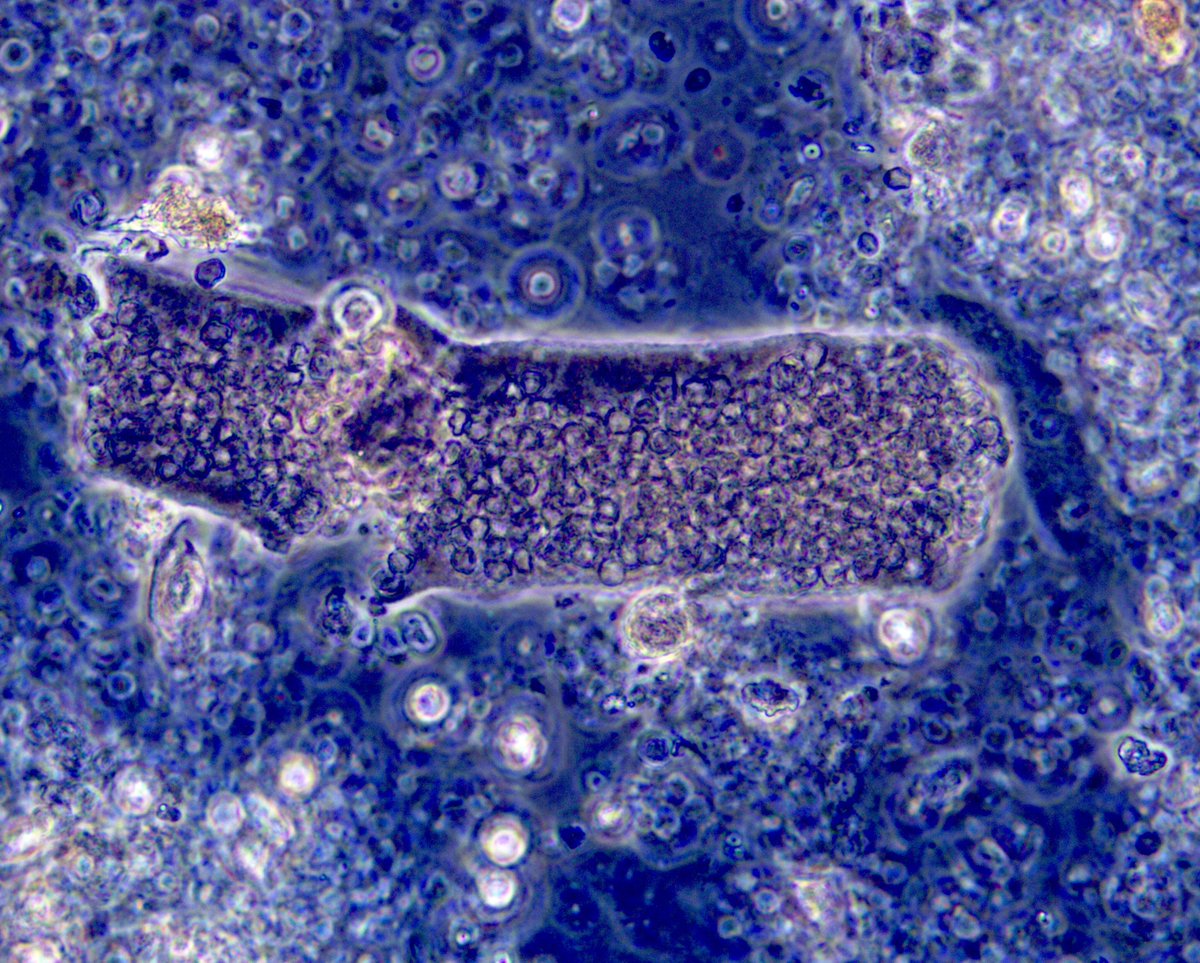
6/x many pigmented (hem) waxy casts are also found, along with dysmorphic RBCs (not quite acanthocytes). So, definitely pointing to acute GN and concomitant tubular injury #UrinarySediment 

7/x so at this point, the h/o MSSA became extremely important, suspicion of infection-related GN must be considered. That day, low grade fever developed. Of course, next step is to get an echocardiogram. Boom, vegetation. 

8/x SBE-GN can lead to crescentic pauci immune or crescentic DPGN. C3 low in ~50% (normal here), +MPO-ANCA (pending here). Back on cefazolin. CT Sx consulted. Kidney biopsy scheduled. We may see this lesion 👇 

9/9 conclusions: 1. Important to avoid cognitive (confirmation) biases; 2. #UrineMicroscopy is a valuable tool; 3. Kidney US is not just to r/o hydro, check size, echogenicity; 4. IVDA+bacteremia+AKI: think SBE-GN
• • •
Missing some Tweet in this thread? You can try to
force a refresh