1/ Can intramuscular vaccination induce an immune response that protects against not only disease (#COVID19), but viral infection and transmission of #SARSCoV2 in the local mucosa? In a new preprint by @GeorgieNahass et al we found that saliva may be KEY🧵
medrxiv.org/cgi/content/sh…
medrxiv.org/cgi/content/sh…
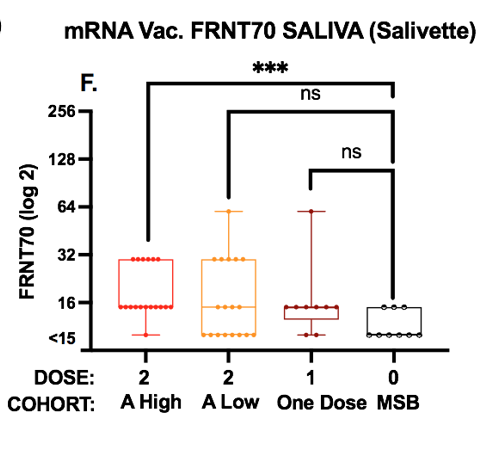
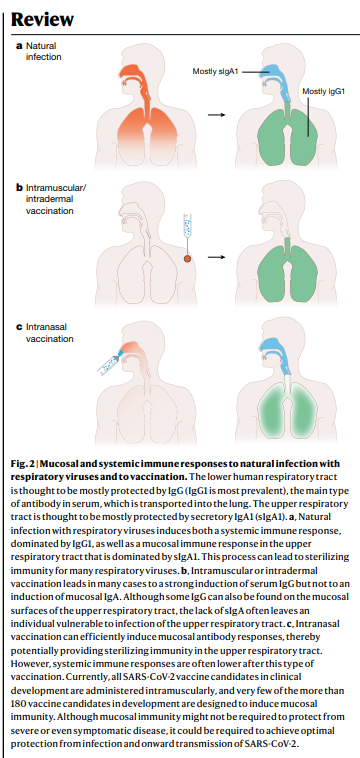
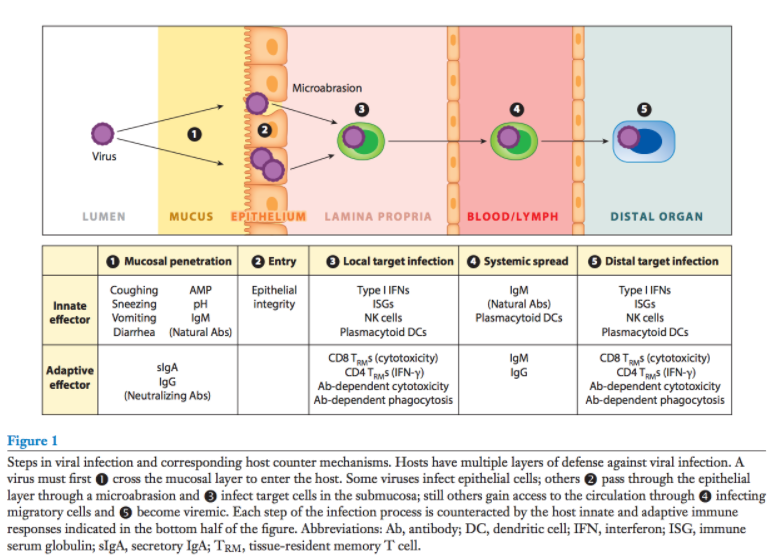
2/ Secreted *mucosal* antibodies 💦 protect from infection or spread of infection in the mucosa of the nose 👃 and mouth 👄. *Circulating* antibodies 🩸prevent systemic infection and disease. Which antibodies do we make after vaccination? @SalivaStudy💉
https://twitter.com/SalivaStudy/status/1332174878326210560?s=20
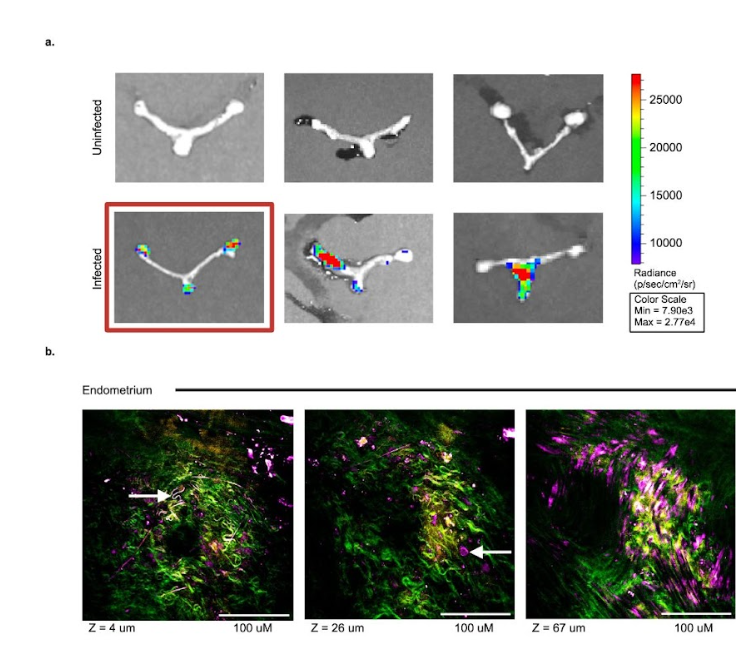
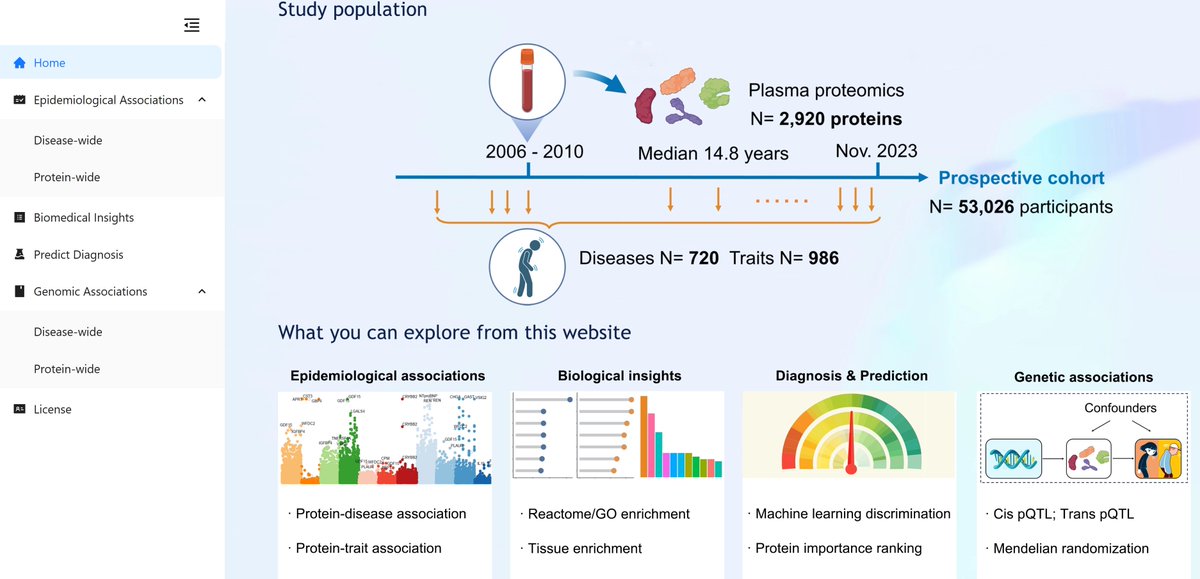
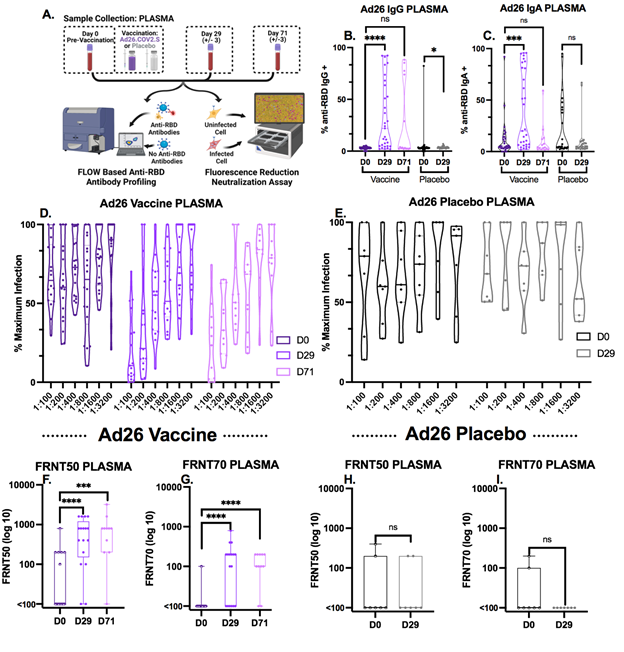
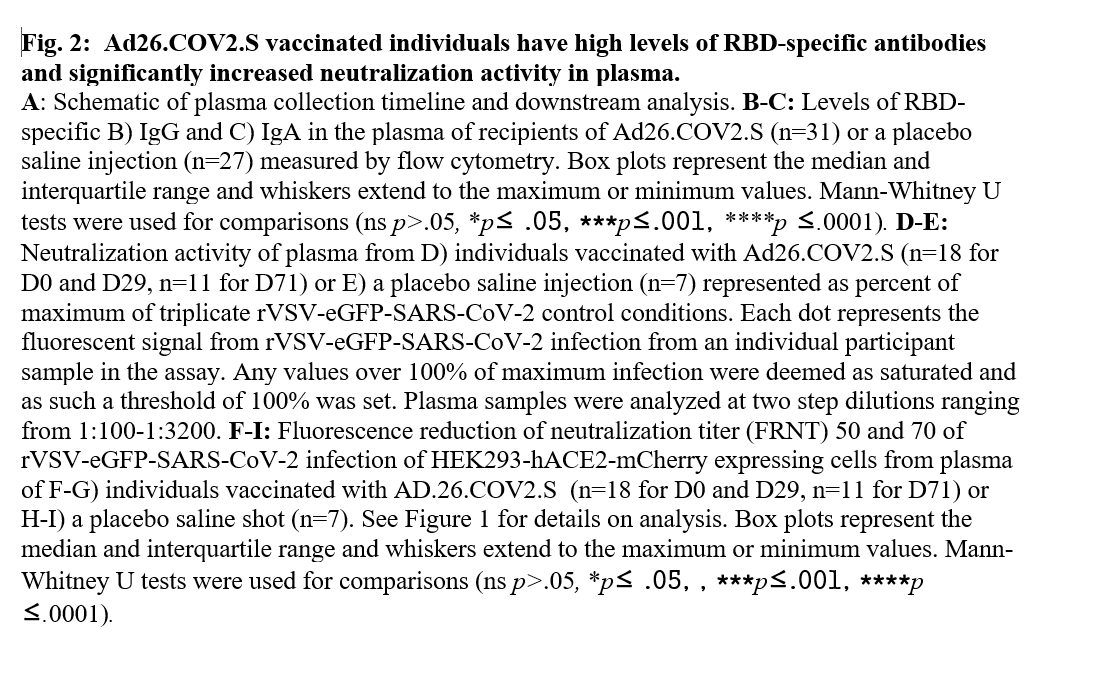
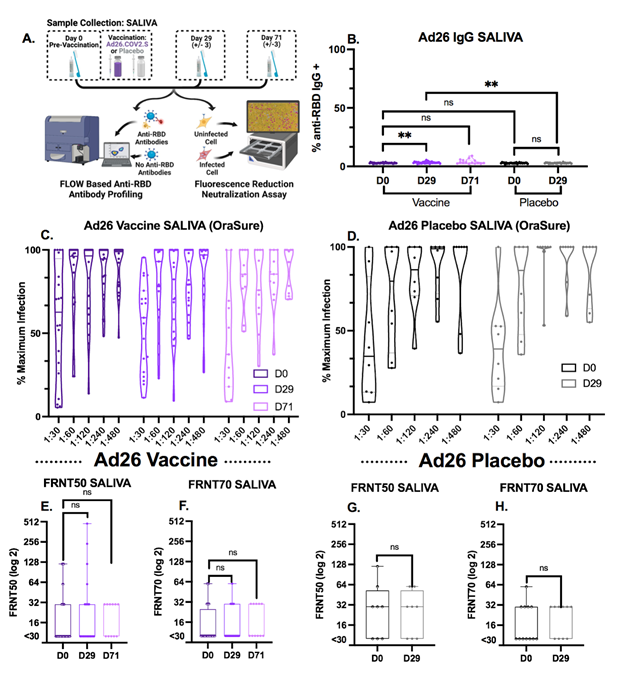
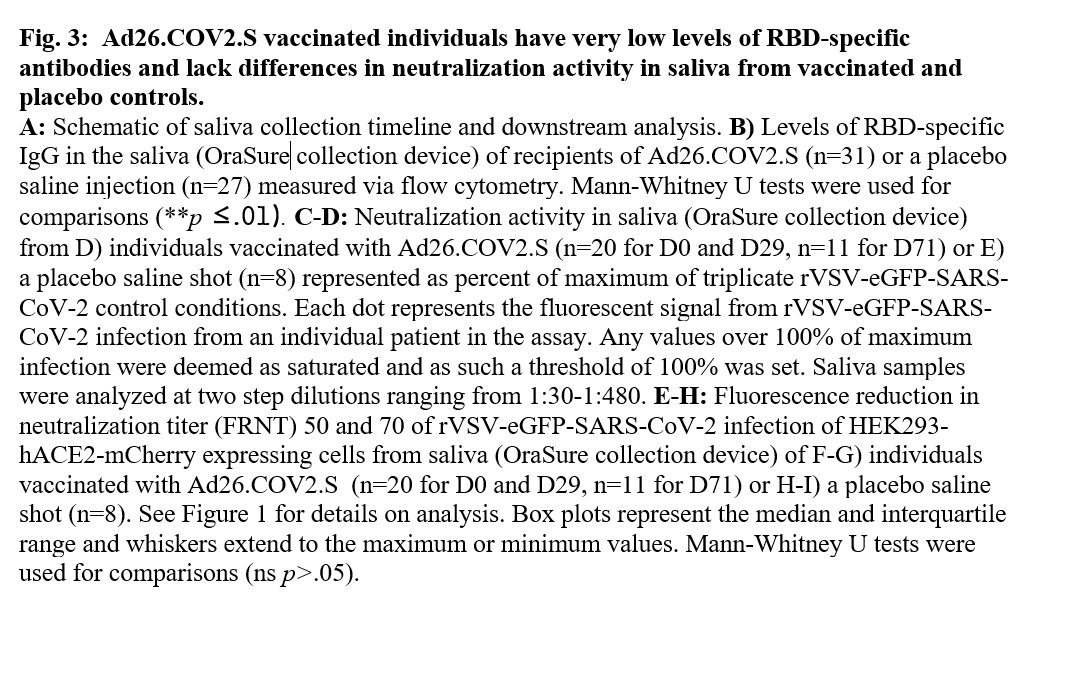
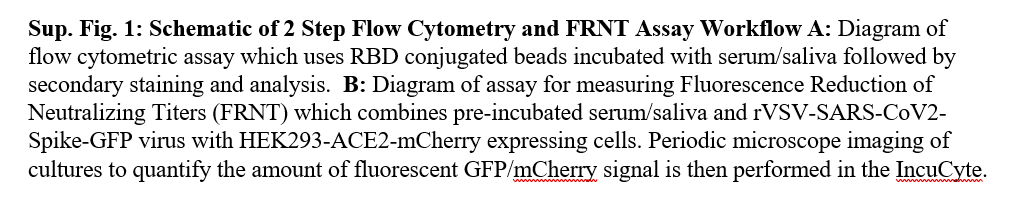
3/ We measured antibodies against the #SARSCoV2 receptor binding domain (RBD) in *plasma* & *saliva* from convalescent or vaccinated individuals and tested their neutralizing potential using a replication competent rVSV-eGFP-SARS-CoV-2.
VIDEO:
#COVID19
VIDEO:
https://twitter.com/ImmunoFever/status/1380246827279151104?s=20
#COVID19
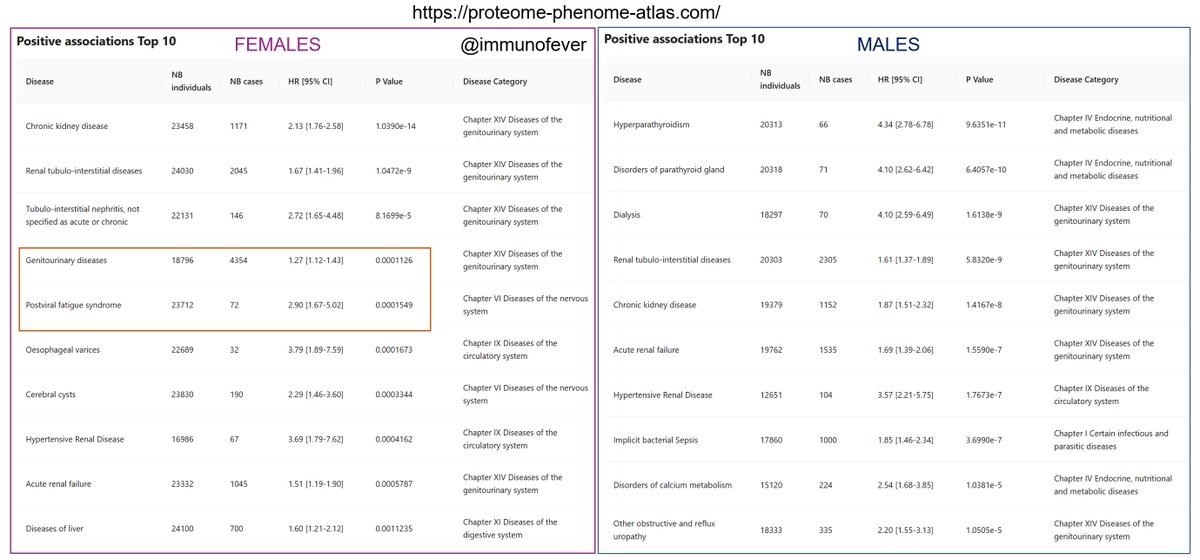
4/ While individuals with a history of #COVID19 had detectable RBD-specific antibodies and neutralizing ability in their *saliva and plasma,* one of our most surprising findings was the striking differences in *salivary* antibodies between vaccines. 🦠💉 


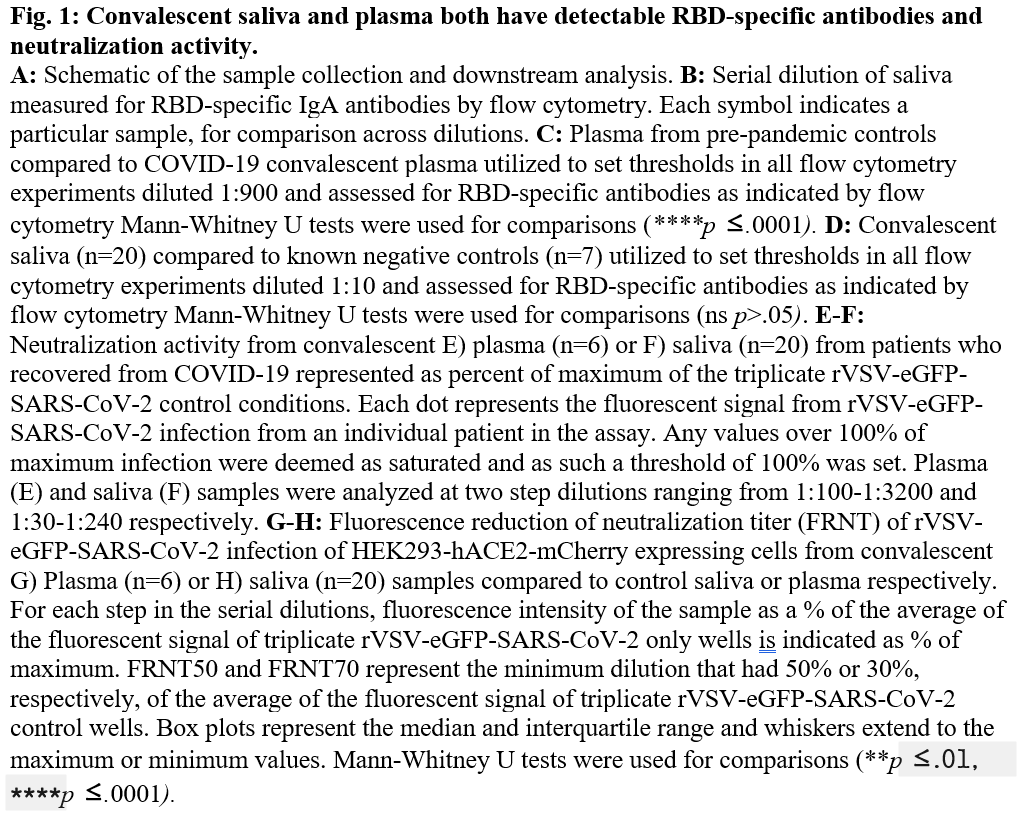
5/ Individuals who had received 1 dose of Ad26.COV2.S (J&J) produced high levels of *circulating* antibodies against RBD, as expected. However, these same individuals had very low levels of antibodies in their *saliva,* which also lacked the ability to neutralize the virus. 💉 



6/ The true ✨magic of #ScienceTwitter is *THIS* right here! The tweet that kicked off an incredible international collaboration to help advance our understanding of our immune responses to these vaccines! @JenGommerman we adore you! 💕
#SpitKingdom
https://twitter.com/JenGommerman/status/1383148261519790090?s=20
#SpitKingdom
7/ Individuals who had received mRNA vaccination with BNT162b2 (Pfizer) or mRNA-1273 (Moderna) in 1 or 2 doses also developed robust RBD-specific antibodies with neutralizing ability in the *plasma* but unexpectedly ALSO in the *saliva.* #COVID19 💉💉 

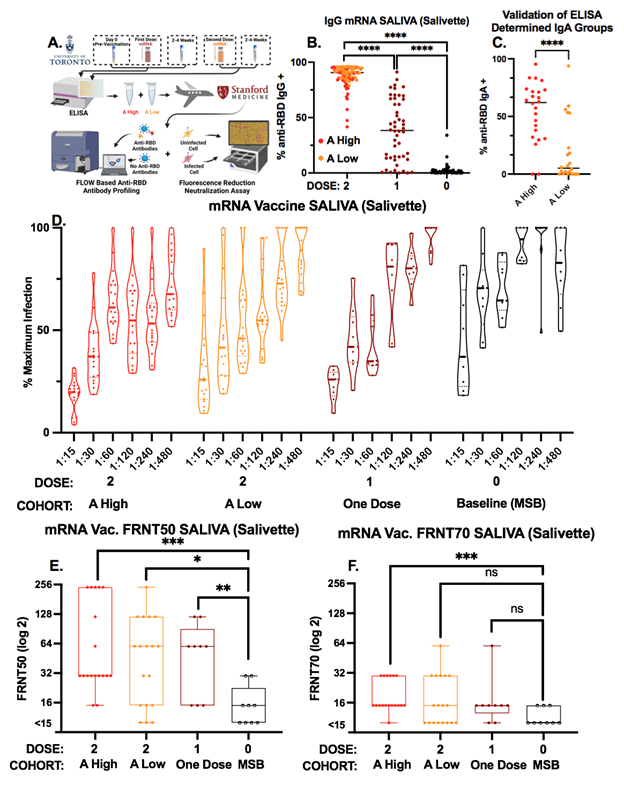
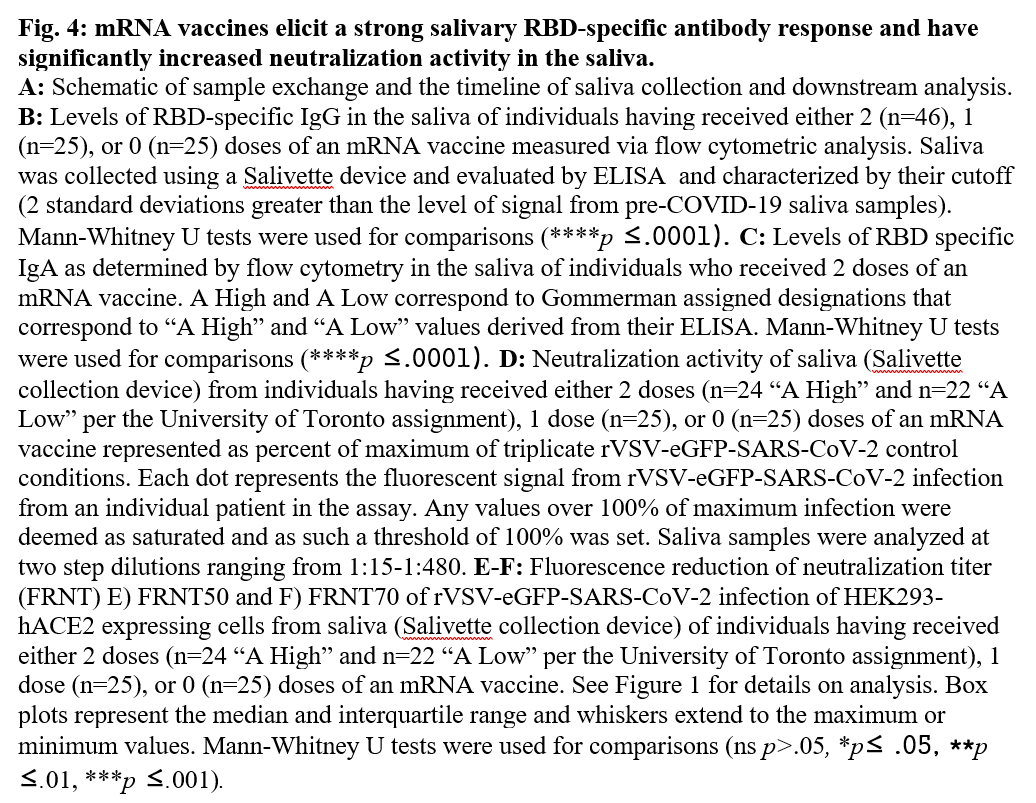
8/ The highest levels of *salivary* neutralizing activity were in participants who received 2 doses of mRNA vaccine AND made high levels of anti-RBD IgA in their saliva (comparable to convalescent individuals). Only cohort to reach statistical significance at stringent FRNT70. 
9/ Dr. @JenGommerman @UofT 🇨🇦 & team evaluated these same *saliva* samples and found that their IgA had secretory chain, demonstrating that these are dimeric IgA (found in mucosal tissues)
PAPER (@SalmaSheikhM et al): medrxiv.org/content/10.110…
THREAD:
PAPER (@SalmaSheikhM et al): medrxiv.org/content/10.110…
THREAD:
https://twitter.com/JenGommerman/status/1423317956197556230?s=20
10/ Most importantly, our study shows that all 3 vaccines granted emergency use authorization (EUA) in the US induce robust antibody response in the *plasma* protecting against severe disease and death. We need every vaccine in our fight against this global threat.💉💉💉 #COVID19 

11/ ALL 3 vaccines w/ EUA approval in the US can induce immune responses in the *saliva,* albeit at varying levels.
Not having sufficient levels of mucosal antibodies at the site of infection (👃&👄) may put people at risk for infection & transmission in the upper airway.
Not having sufficient levels of mucosal antibodies at the site of infection (👃&👄) may put people at risk for infection & transmission in the upper airway.
12/ Could there be a novel mechanism of the mRNA vehicle to permeate the mucosal immune compartment and induce a mucosal immune response? This has not historically been seen with intramuscular vaccination.
PHOTO: @FlorianKrammer @Nature nature.com/articles/s4158…
PHOTO: @FlorianKrammer @Nature nature.com/articles/s4158…
13/ Or is it just leakage of antibodies from the blood into the saliva, where super high antibody levels in the blood then also lead to more significant levels in the saliva? 
14/The role of *salivary* antibodies in protection against #SARSCoV2 is unknown. Surveillance of salivary antibodies could provide critical insight into who is at highest risk for breakthrough infection post vaccination, as well as helping to optimize protection against the virus 
15/ The immune response is complex and multifaceted. Our study was restricted to the role of antibodies. T-cells were not evaluated, although they may play a role that is especially important in protection against severe disease resulting from new variants. #COVID19 #COVID 

16/ Together, our 2 studies provide extremely pertinent new information on the impact of different vaccine platforms, dosing, and schedules on mucosal immunity to #SARSCoV2, and compare different vaccination strategies that have been implemented in North America.💉🇺🇸🇨🇦 #COVID19 

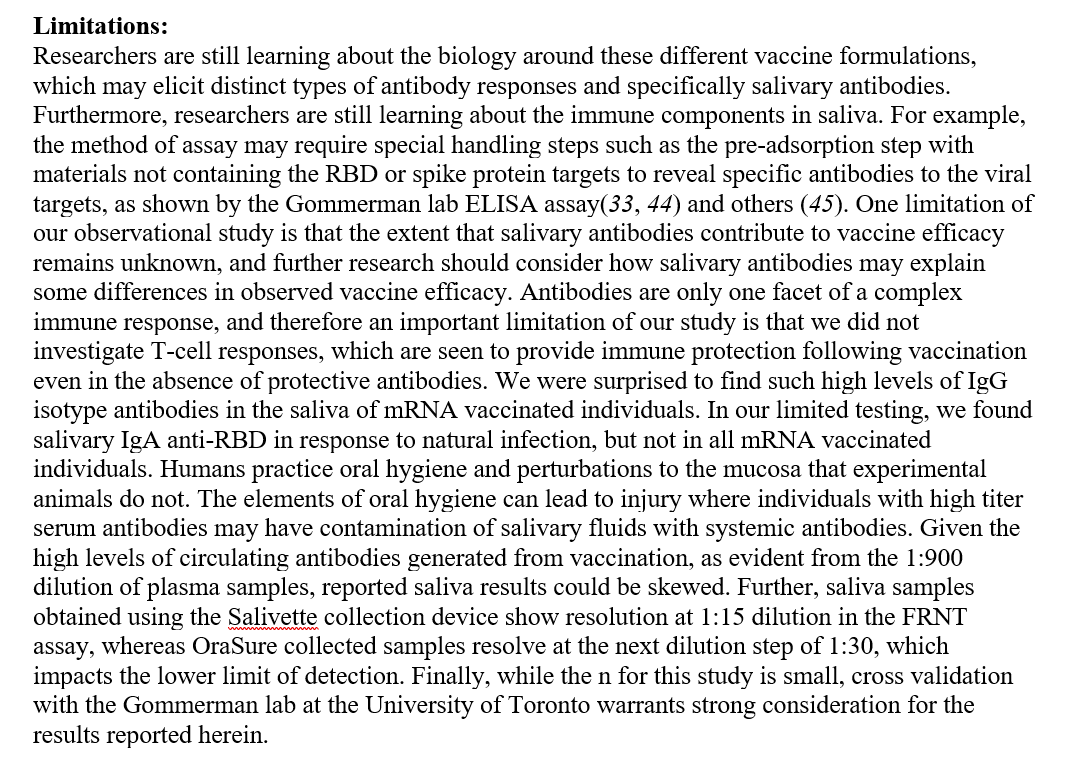
17/ Our study has several limitations, notably, this data is PRE-DELTA. The sample sizes are small. ***
We tried to capture as many of the limitations as we could think of in the text.
We tried to capture as many of the limitations as we could think of in the text.
18/ We would like to thank all of the co-authors @GeorgieNahass @ShulmanSalomon @ErinSandersNP (+many not on twitter) for all your efforts and contributions, and so many of you science twitter friends for helpful advice and reagents @CyrilPedia @KevinWNg @sding88 @vsv512
@threadreaderapp unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh