1/ Merry #TweetorialTuesday to all our #MedEdTwagTeam, #MedEd, and #MedTwitter friends!
Today we will be chatting about how to fit in teaching when on an #InpatientTeaching service.
Today we will be chatting about how to fit in teaching when on an #InpatientTeaching service.

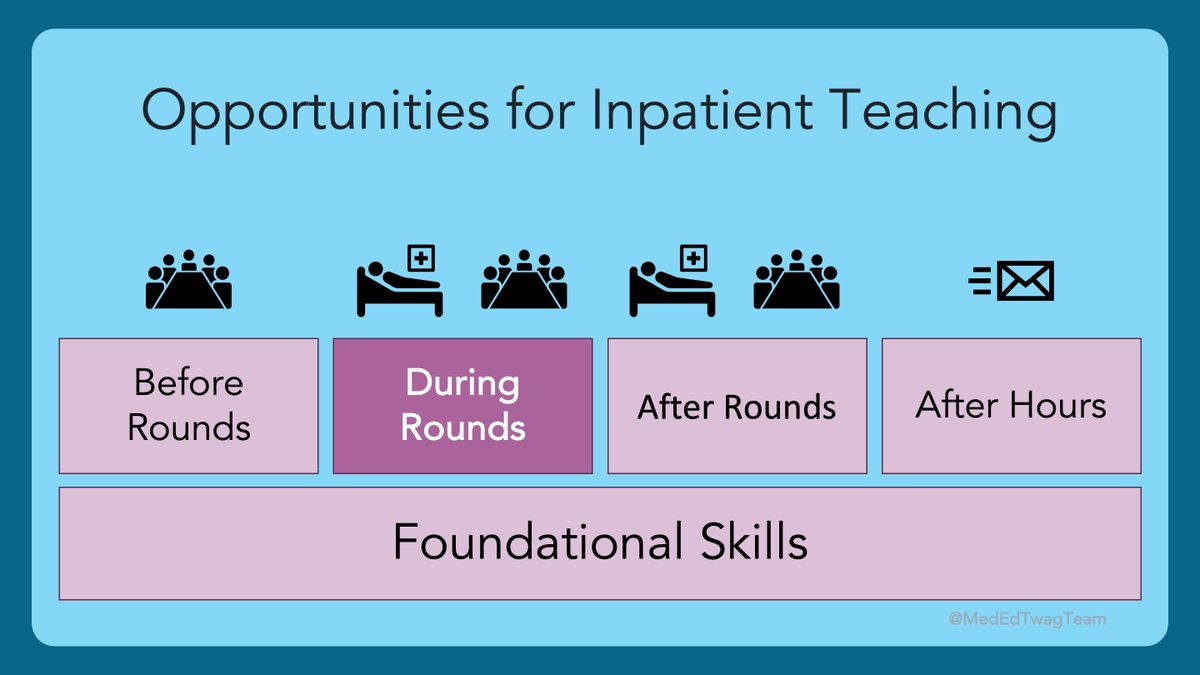
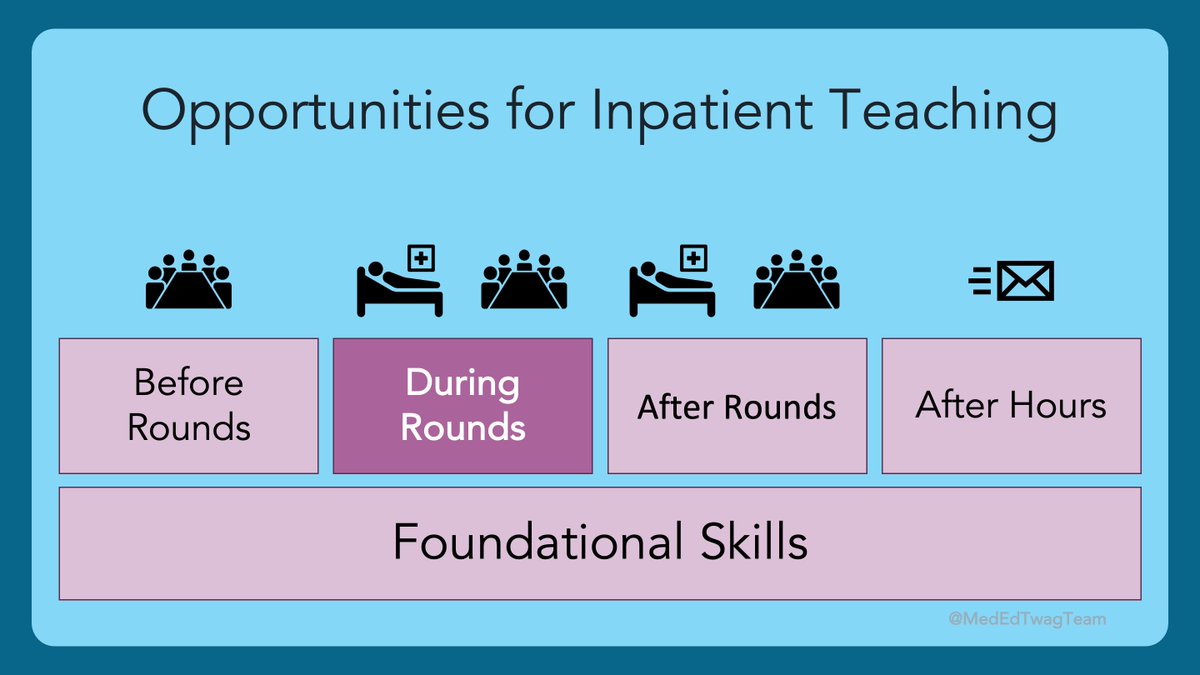
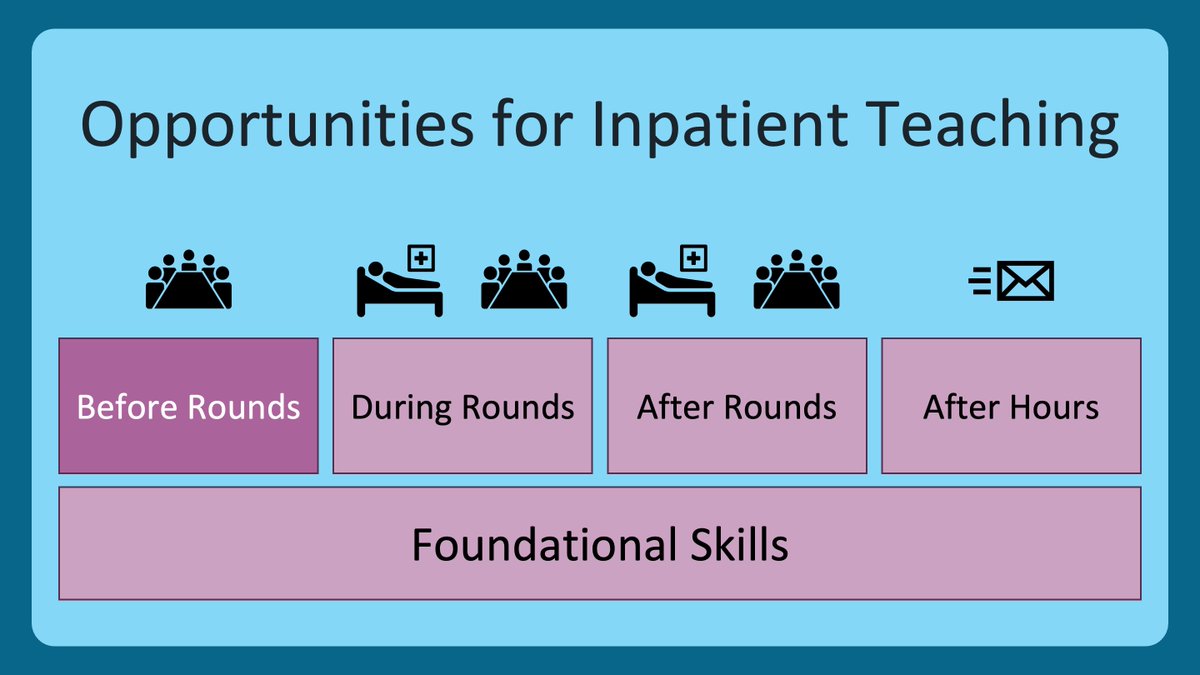
2/ As @JenniferSpicer4 outlined two weeks ago, we are going to structure our upcoming content in terms of different times when teaching can occur.
However, today is going to be an overview of structuring one’s day, and is part of our foundational skills section.
However, today is going to be an overview of structuring one’s day, and is part of our foundational skills section.

3/ And, as with all #MedEd, what I do will NOT translate directly to your practice, as learning contexts are so unique and specific. However, the big ideas and concepts are transferrable.
4/ Before we talk about what I do, we need to talk about rounds. What are they for?
A pair of papers in @JHospMedicine and @JournalofGME provide an excellent conceptualization.
Thanks #IRL friends: @jeannemfarnan, @BradMonash, Drs. Barrett Fromme & Alekist Quach (I 👀 you)
A pair of papers in @JHospMedicine and @JournalofGME provide an excellent conceptualization.
Thanks #IRL friends: @jeannemfarnan, @BradMonash, Drs. Barrett Fromme & Alekist Quach (I 👀 you)
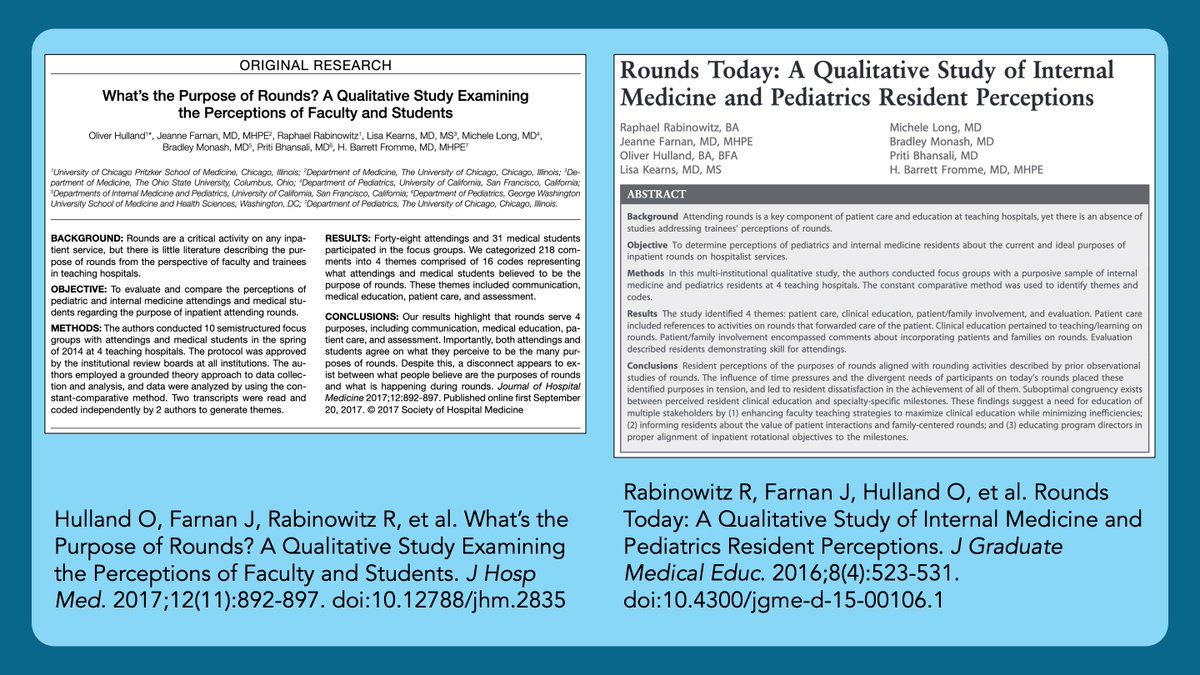
5/ Both papers found the same 4 categories of purposes for rounds with 1 major difference:
🔑Attendings & Students thought that rounds were effective at achieving all 4 things.
🔑Residents felt patient care discussions dominated rounds, leaving little time for other objectives.
🔑Attendings & Students thought that rounds were effective at achieving all 4 things.
🔑Residents felt patient care discussions dominated rounds, leaving little time for other objectives.

6/ With the "work vs. learning paradigm" in mind, here is how I structure a typical day for myself, residents, and students.
For context, I am a hospitalist at a VA hospital.
For context, I am a hospitalist at a VA hospital.

7/ I dedicate only 90 minutes to rounds.
The expectation I set is we will see as many patients as we can, but a typical team (census 10-16) sees 4-6 patients in those 90 minutes.
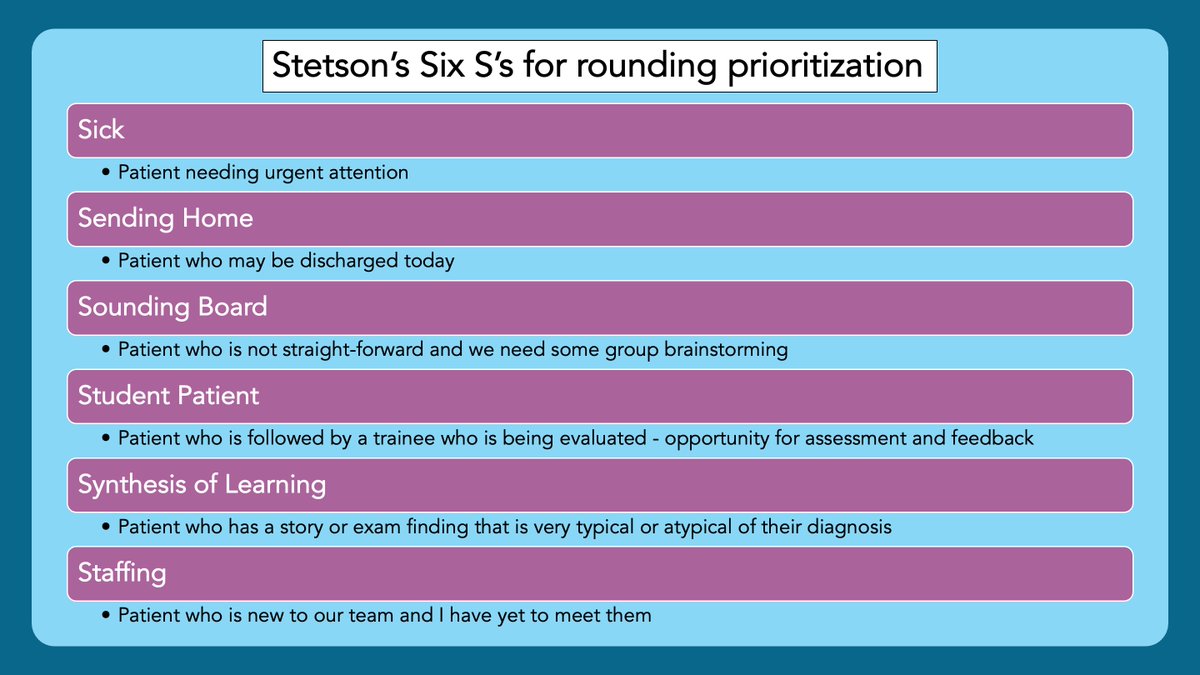
👇 are the criteria (mostly in order) that I introduce to help prioritize who we see as a team.
The expectation I set is we will see as many patients as we can, but a typical team (census 10-16) sees 4-6 patients in those 90 minutes.
👇 are the criteria (mostly in order) that I introduce to help prioritize who we see as a team.
8/ But, wait, Geoff! You don’t see all patients as a team?
No. No, I don’t. I have to see all the patients, but the learners don’t. By capping rounds, we can be efficient, focus on learning, and get back to work at a reasonable time. Here is how I think about 90-minute rounds:
No. No, I don’t. I have to see all the patients, but the learners don’t. By capping rounds, we can be efficient, focus on learning, and get back to work at a reasonable time. Here is how I think about 90-minute rounds:

9/ A couple caveats:
✅On post-call days, when there are 6-9 new patients, the 90-minute cap doesn’t apply.
✅If there is still excellent learning remaining after the 90 minutes, anyone (typically students) can see more patients with me.
✅On post-call days, when there are 6-9 new patients, the 90-minute cap doesn’t apply.
✅If there is still excellent learning remaining after the 90 minutes, anyone (typically students) can see more patients with me.
10/ So here is how I ”fit it in”. In yellow, you can see all the formal teaching/learning opportunities.
That 11:30 slot is when I get to give a chalk-talk, review some literature, debrief the learning pearls of the week, help a trainee teach, etc.
That 11:30 slot is when I get to give a chalk-talk, review some literature, debrief the learning pearls of the week, help a trainee teach, etc.

11/ The key to effective 90-minute rounds is solid AM chart review. I skip morning report to do this. If this isn’t possible for you, you’ll need to find other time to do this. This is essential for shortened rounds to work. 
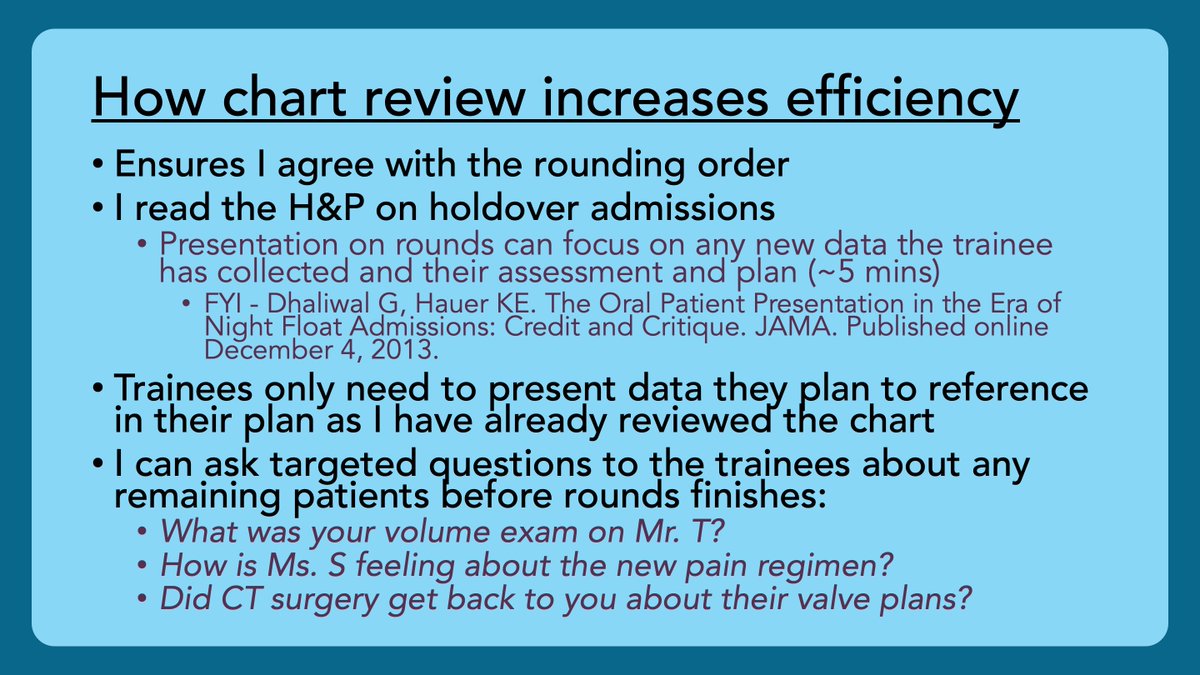
12/ NOTE: I communicate to my team on day 1 that I will be doing chart review every AM to ensure that rounds are efficient & are spent learning & problem solving, rather than communicating information that can be found in the EMR. All my trainees have given this 👍👍
13/ How do you all fit it in? What are your thoughts on 90-minute rounds? What about the 6 S’s? What about not seeing all the patients as a team?
This approach works really well in my context. Would LOVE to hear what works well in yours.
This approach works really well in my context. Would LOVE to hear what works well in yours.
14/ Next week, stay tuned for @JenniferSpicer4 giving her take on this theme from the sub-specialty perspective.
In the meantime, make sure you are following Dr. Spicer, @GStetsonMD, @MedEdTwagTeam, and our newest member, @YihanYangMD!
Tweet you next week!
In the meantime, make sure you are following Dr. Spicer, @GStetsonMD, @MedEdTwagTeam, and our newest member, @YihanYangMD!
Tweet you next week!

• • •
Missing some Tweet in this thread? You can try to
force a refresh