
1/New study in @DrugAlcoholDep finds that a national Stay-at-Home order for COVID-19 had "variable" impacts on opioid OD-
And it demonstrates that Emergency Dept overdose diagnoses deliver only a very cloudy view on overdose rates, - KY, OH, MA, NY sciencedirect.com/science/articl…!
And it demonstrates that Emergency Dept overdose diagnoses deliver only a very cloudy view on overdose rates, - KY, OH, MA, NY sciencedirect.com/science/articl…!

2/ 3 of 4 states (MA,NY,OH,*not KY*) had a 10 week ⬇️ in ED visits for opioid OD after pandemic hit.
Then, ED visits ⬆️ for MA,OH,KY
**But ED visits don't relate tightly to death**
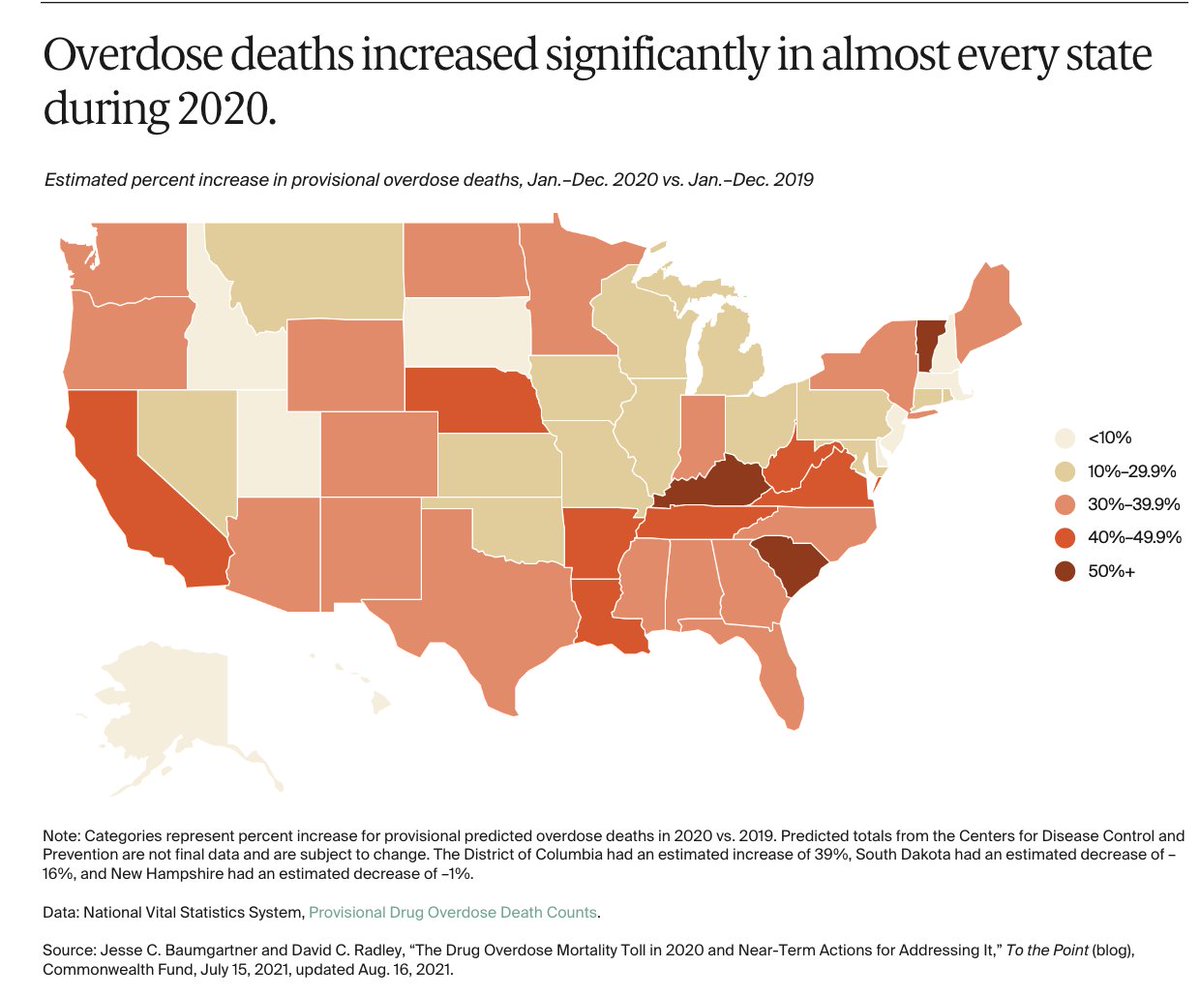
OD deaths for 2020, relative to 2019:
MA:⬆️2%
NY:⬆️34%
KY:⬆️54%
OH:⬆️22%
commonwealthfund.org/blog/2021/drug…
Then, ED visits ⬆️ for MA,OH,KY
**But ED visits don't relate tightly to death**
OD deaths for 2020, relative to 2019:
MA:⬆️2%
NY:⬆️34%
KY:⬆️54%
OH:⬆️22%
commonwealthfund.org/blog/2021/drug…
3/Authors conclude what I agree with, but I'll comment.
They say:
"results support our hypothesis of a significant impact of the national stay-at-home order on ED encounters for suspected OOD in the 4 HCS states, but indicate that the dynamics of this impact differed"
YES, and.
They say:
"results support our hypothesis of a significant impact of the national stay-at-home order on ED encounters for suspected OOD in the 4 HCS states, but indicate that the dynamics of this impact differed"
YES, and.
4/As the authors say: when care systems were overwhelmed, that suppressed care-seeking, but only for a few weeks in MA
Much more variation - mostly unexplained- is going on here:
Much more variation - mostly unexplained- is going on here:

5/We face real flaws in use of "Overdose Syndromic surveillance" using hospital &emergency department visits
Such data underdetect OD or are biased, in mostly unknowable ways, by variations in
*care-seeking
*fatality related to variations in drug supply
*poor diagnostic coding
Such data underdetect OD or are biased, in mostly unknowable ways, by variations in
*care-seeking
*fatality related to variations in drug supply
*poor diagnostic coding
6/This also means that most prescription opioid risk calibration and monitoring tools - useful as they may be (and I personally rely on VA's STORM tool) - over-emphasize ONE subset of overdose and/or suicide events: the ones patients seek care for.
7/If our goal is monitoring health, we will *never have a perfect solution*
But we should supplement health system monitoring with **community surveys** to assess the prevalence of overdose
Our wonderful Birmingham research team has new data soon (+@ChelseaLShover
and others!)
But we should supplement health system monitoring with **community surveys** to assess the prevalence of overdose
Our wonderful Birmingham research team has new data soon (+@ChelseaLShover
and others!)

• • •
Missing some Tweet in this thread? You can try to
force a refresh






