1/A new JAMA paper by @AliciaAgnoli & @fenton_jj finds #opioid taper associated with ⬆️risk of overdose & mental health crises in patients previously on higher opioid doses. I’ll offer context, summarize findings, and review implications. Here goes. jamanetwork.com/journals/jama/…
2/Context: prior data showed ODs more likely in patients with higher Rx’d dose, which *couldn’t prove* cause & effect. MDs had historically ⬆️’d dose in patients who had other risks. One can argue that ⬆️doses
*ADDED risk,
*or were MARKERS of risk:
jamanetwork.com/journals/jama/…
*ADDED risk,
*or were MARKERS of risk:
jamanetwork.com/journals/jama/…
3/An example: I had a case where the prior MD ⬆️’d opioid dose for a long-term patient who reported ⬆️pain. But that pt had long-term psych diagnoses, and pain ⬆️ *right after his son died* Thus, the dose ⬆️was a marker for emotional risk factors, AND (b) dose may have added risk
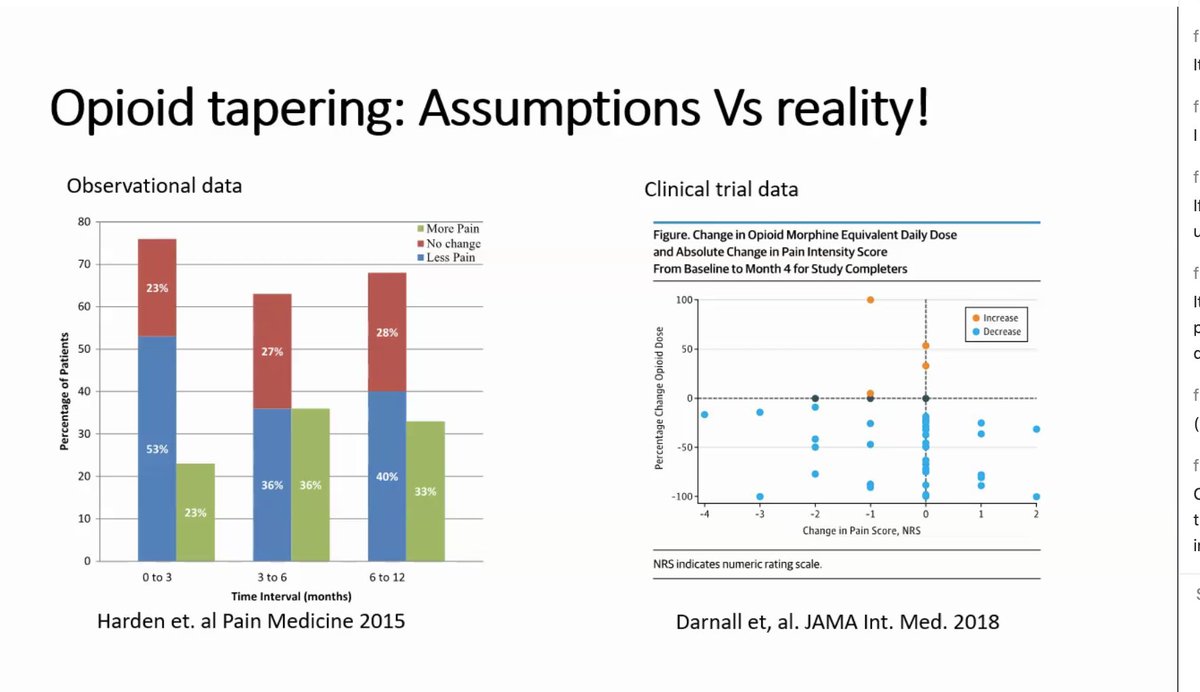
4/By 2017, policies outran evidence. SUPPORT Act mandates dose limits in Medicaid.
80 experts urged @NCQA *not* to enshrine dose ceilings “that could actually increase risk to patients”. We failed. Such metrics are used by payers & legal investigators: stefankertesz.medium.com/an-opioid-qual…
80 experts urged @NCQA *not* to enshrine dose ceilings “that could actually increase risk to patients”. We failed. Such metrics are used by payers & legal investigators: stefankertesz.medium.com/an-opioid-qual…

5/Crucially, despite that pressure to push doses down, there *never was* any research (observational or trial data) to show that pushing each patient’s dose ⬇️made that patient safer. This is not a good way to guide practice.
6/Many of us saw patients traumatized by dose reduction. Some of us were called to help. My colleagues & I reported the harms, publicly and privately. So did other experts, like this letter led by @BethDarnall: academic.oup.com/painmedicine/a…
7/Plenty of large database research studies set the stage for this new report from @AliciaAgnoli. Data show that abrupt opioid discontinuations became more frequent in Medicare, despite FDA warnings against it. Here, from @Hneprash and @ml_barnett pubmed.ncbi.nlm.nih.gov/33515197/
8/A series of studies found associations between dose reduction and termination of care, ODs, & suicides. The largest (a VA study I helped initiate) showed ⬆️risk of OD & suicide deaths. And yes, it had limitations, which I helped explain here:
https://twitter.com/StefanKertesz/status/1235652849998032896?s=20
9/And since I detest oversimplification, let's note: dose reductions can also be helpful for *some patients*. Some studies show pain is NOT worse, on statistical average, or improves, with intentional care in voluntary patients. Nice review here: pubmed.ncbi.nlm.nih.gov/33145689/
10/The new JAMA study is big. It has a commercial/Medicare population. Patients included if dose > 50 mg (2007-2019). Among 113,618 persons, 30% had “taper” = decline in >15% relative to a baseline. The main comparisons are of “periods not tapered” to “periods of taper” 

11/The outcomes studied were emergency or hospital care for drug OD/withdrawal and, separately, and mental crises. Analyses appropriately adjust for age, baseline opioid dose, medical & psychiatric conditions, co-prescribed benzodiazepines, prior ODs & more
12/The data show: greater drug overdose (and withdrawal) event frequency for periods following taper compared to no taper. The higher the dose at the outset, the bigger that increment in risk (my graphic, from Table 2) 

13/The data show: greater mental health crises event frequency for periods following taper compared to no taper. The higher the dose at the outset, the bigger that increase in risk (my graphic, from Table 2) 

14/A higher speed of taper (“velocity”) was associated with *additional increment in risk* of poor outcome. But there was no hint that slow velocity of tapering was associated with lower incidence of OD or mental health crisis, relative to not tapering.
15/Also: this study outcome is NOT “death”.It focuses on encounters for OD/withdrawal or mental crisis.This has advantages: it avoids some statistical biases that may have affected our VA study on death. But it could underestimate adverse events, as people may not seek care.
16/Does this *prove cause and effect*? The authors& editorial by @PoojaLagisetty @Amy_Bohnert @LarochelleMark are properly cautious. Large databases can’t show reasons for taper, whether it was wanted or how it was done. That applies to all prior studies of Rx dose & risk, too.
17/Implications: Frontline clinicians (like me) may struggle both with (a) system-level pressures that make us fearful in prescribing, even for patients doing well on opioids & (b)patients on opioids doing poorly, apparently dependent, sometimes confrontational.
18/For frontline clinicians seeing patients struggling, there are competing views:
should we fully Reassess? Offer new psychological care? Propose tapering? Continue opioids but see patient more often?
Y’all are INVITED to weigh in on here, but let me mention my principle:
should we fully Reassess? Offer new psychological care? Propose tapering? Continue opioids but see patient more often?
Y’all are INVITED to weigh in on here, but let me mention my principle:
19/My approach: listen for a patient’s full history (context). Get advice from pharmacists, nurses, colleagues. I talk with patients, explain what I know & don’t know. It’s crucial to avoid *bulldozing* patients:
Our podcast “Forced Opioid Taper” pod.link/healer/episode…
Our podcast “Forced Opioid Taper” pod.link/healer/episode…
20/On our policies: evidence shows we must reverse pressures currently enshrined in payer policies, quality metrics, legal investigation thresholds, and law (SUPPORT). These mandates are *not justified clinically or ethically*. Yes, we published that:
https://twitter.com/StefanKertesz/status/1280996765798469632?s=20
21/As research priority, my team seeks to understand, document, & fix the factors at play when where Rx stoppage is implicated in the death by suicide. @AllysonVarley @PainPtFightBack a team of suicidologists & I are recruiting for our pilot: go.uab.edu/csiopioids. 

21/Broadly, research on pain care needs to move beyond focus on “the pills”. Of course, opioids were oversold. But right now, a focus on “the pills" is interfering with our attempts to see human beings with pain as whole people, and it spurs abandonment. jamanetwork.com/journals/jaman…
22/ Feedback invite: Anyone working hard to help people with pain, but sees things differently from me? Chime in!
But hear this: if part of your current income $ is based on *serving as an expert witness in opioid litigation with billions of dollars at stake*,
disclose it 😉
But hear this: if part of your current income $ is based on *serving as an expert witness in opioid litigation with billions of dollars at stake*,
disclose it 😉
23/What I wrote is my effort to encompass a matter where I have studied the research, published in it, and worked the front lines as prescriber and risk mitigator.
I invite patients to comment.
It’s *your lives* at stake here
I invite @AliciaAgnoli to add insight about her work
I invite patients to comment.
It’s *your lives* at stake here
I invite @AliciaAgnoli to add insight about her work
24/Finally: for anyone hungry for insight on medical care as a matter of healing relationships and not just technocratic decisions, check out our podcast: “On Becoming a Healer” (on all platforms). Our most recent episode touches on racism: pod.link/healer /END
25/Correction, I goofed up the Twitter Handle for Dr. Agnoli: @alicia_agnoli
• • •
Missing some Tweet in this thread? You can try to
force a refresh