1/ Time for #TweetorialTuesday from the @MedEdTwagTeam for our #MedTwitter & #MedEd friends!
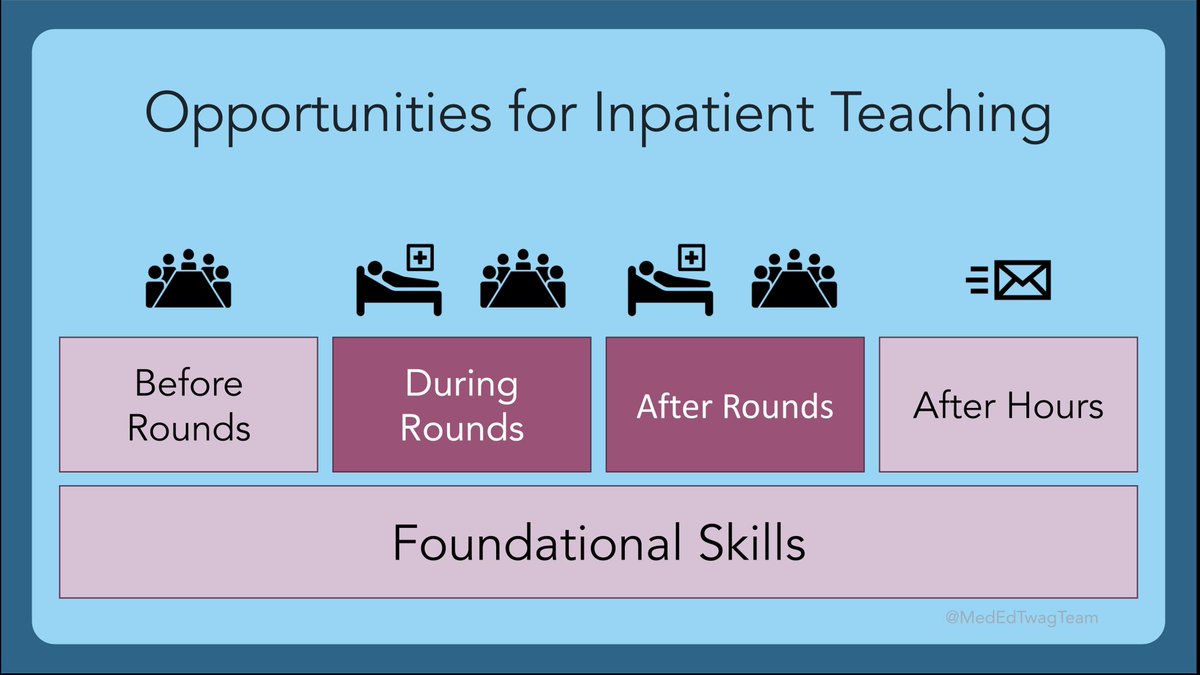
This week is our 3rd “Fitting it All In” on how we structure teaching into our inpatient attending time!
This week is our 3rd “Fitting it All In” on how we structure teaching into our inpatient attending time!

2/ As a reminder, we are discussing the foundational skills for inpatient teaching.
Last week, @JenniferSpicer4 provided her take as a consult service attending:
Last week, @JenniferSpicer4 provided her take as a consult service attending:
https://twitter.com/jenniferspicer4/status/1435281263896760325?s=21https://t.co/12hjMWAnfW

3/ Rounding & teaching on the inpatient service often needs to be adjusted to fit differences in resident schedules & program cultures. Since I’ve been at 2 different institutions recently, I’ll provide a unique perspective on how I’ve changed rounding based on those factors. 

4/ Let’s start!
One practice that has remained consistent for me: before I even start on service, I try to avoid overcommitting myself. I:
[x] Schedule meetings & other commitments to when I’m not on service
[x] Set automated “on service” email reply
One practice that has remained consistent for me: before I even start on service, I try to avoid overcommitting myself. I:
[x] Schedule meetings & other commitments to when I’m not on service
[x] Set automated “on service” email reply

5/ In terms of rounds, some of you know that I prefer bedside rounds, which I use to advance pt care, communicate w/ pts & staff, educate learners & pts.
Bedside rounding allows me to informally assess clinical & communication skills w/ more opportunities for direct observation.
Bedside rounding allows me to informally assess clinical & communication skills w/ more opportunities for direct observation.

6/ For more tips on how to structure bedside teaching, please see my Bedside Teaching #MedEdMethodsMonday Moment: twitter.com/i/events/14376…
The rest of the tweets here will review how I schedule my day.
The rest of the tweets here will review how I schedule my day.

7/ I started attending @ a program where residents had similar schedules daily on wards.
Team: 1 attending: resident: intern & 10pt cap.
Program culture: round w/ team on all pts, admits b4 5PM typically staffed same day.
Afternoon rounds: for pts who require additional TLC.
Team: 1 attending: resident: intern & 10pt cap.
Program culture: round w/ team on all pts, admits b4 5PM typically staffed same day.
Afternoon rounds: for pts who require additional TLC.

8/ Last year, I moved to an institution with:
- 4-day call cycle, q4 28hr call
- variable presence of learners daily
- very medically complex pts
- still 1 attending: resident: intern; 10pt cap
Me trying to figure out how best to teach in this structure when I first started:
- 4-day call cycle, q4 28hr call
- variable presence of learners daily
- very medically complex pts
- still 1 attending: resident: intern; 10pt cap
Me trying to figure out how best to teach in this structure when I first started:
9/ So here is how I adjusted my rounding & teaching time based upon the call cycle & which learners are present each day.
*I use chart-stimulated recall to review H&Ps, progress notes, d/c summaries. Stay tuned to future #MedEdTwagTeam tweetorial on this topic!
*I use chart-stimulated recall to review H&Ps, progress notes, d/c summaries. Stay tuned to future #MedEdTwagTeam tweetorial on this topic!

10/ Bedside rounds aren’t the norm here. Initially, I was hesitant to have teams adopt this practice. But after my 1st year w/ redundant conversations & hx gathering that could’ve been done 1x in the room, I recommitted.
Hopefully I’ve converted some residents @uw_chiefs :)
Hopefully I’ve converted some residents @uw_chiefs :)
11/ I also adjust rounds based on the independence of the PGY3.
Towards the end of the year, many PGY3s want more autonomy. I often schedule 1 day where the team rounds w/out me. The PGY3 then card flips w/ me after, where we also debrief & review teaching/rounding challenges
Towards the end of the year, many PGY3s want more autonomy. I often schedule 1 day where the team rounds w/out me. The PGY3 then card flips w/ me after, where we also debrief & review teaching/rounding challenges
12/ Have others adjusted their rounding/teaching strategies over time? Or after changing jobs?
Next wk, stay tuned for #TweetorialTuesday by @JenniferSpicer4 w/ tips on Preparing for Teaching.
In the meantime, follow @GStetsonMD & @JenniferSpicer4 @MedEdTwagTeam!
Next wk, stay tuned for #TweetorialTuesday by @JenniferSpicer4 w/ tips on Preparing for Teaching.
In the meantime, follow @GStetsonMD & @JenniferSpicer4 @MedEdTwagTeam!
• • •
Missing some Tweet in this thread? You can try to
force a refresh