oh, the life & times of remdesivir! - let's review the bizarre trajectory we've taken with this medication! with emoji's to represent each study 🤣
we start with a retrospective series of patients treated with remdesivir under the banner of "compassionate use." most patients didn't die. this paper has so many flaws, at this point it's merely a case study in horrific research design 🤮 (commentary: bit.ly/2XBwnx1) 

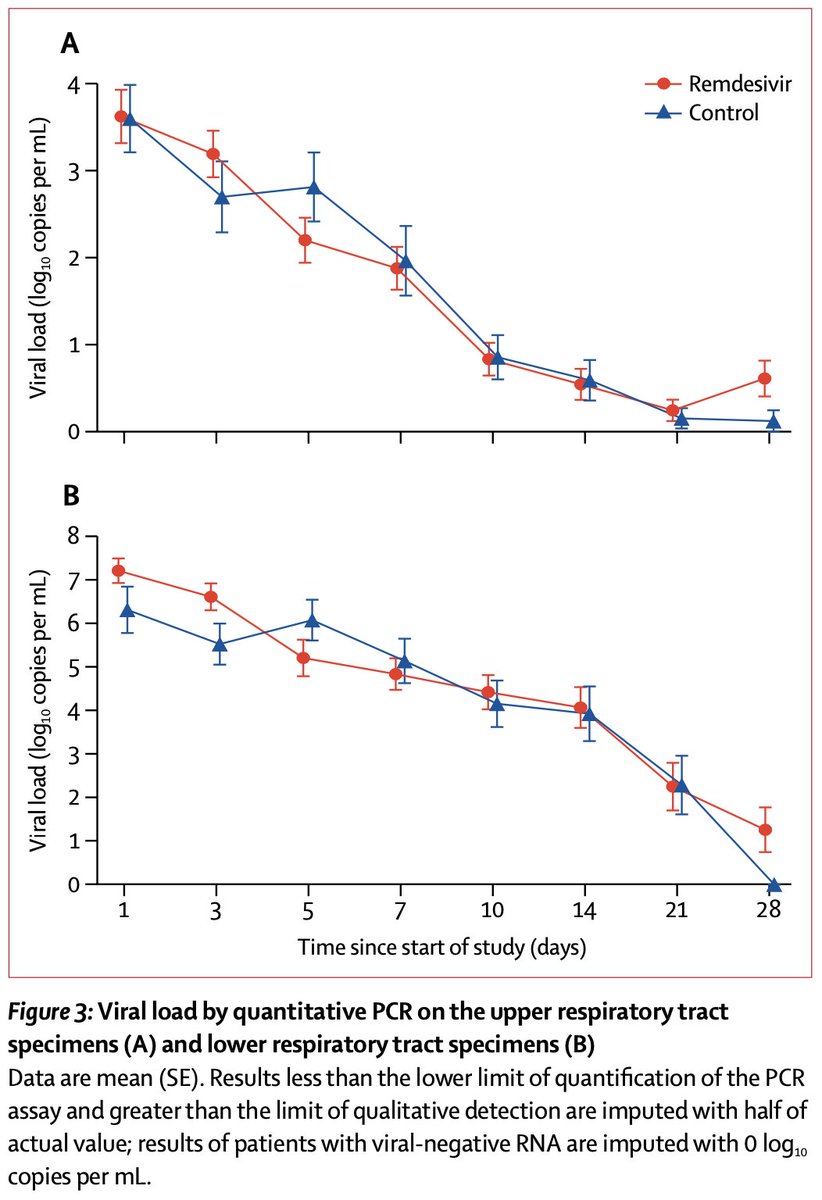
next: the 1st placebo-controlled trial. the primary endpoint (time to clinical improvement) was negative, as were most 2nd endpoints (including viral load). the only glimmer of benefit was faster clinical improvement in one slicing of the data 🥴 (bit.ly/3lIxnXZ) 




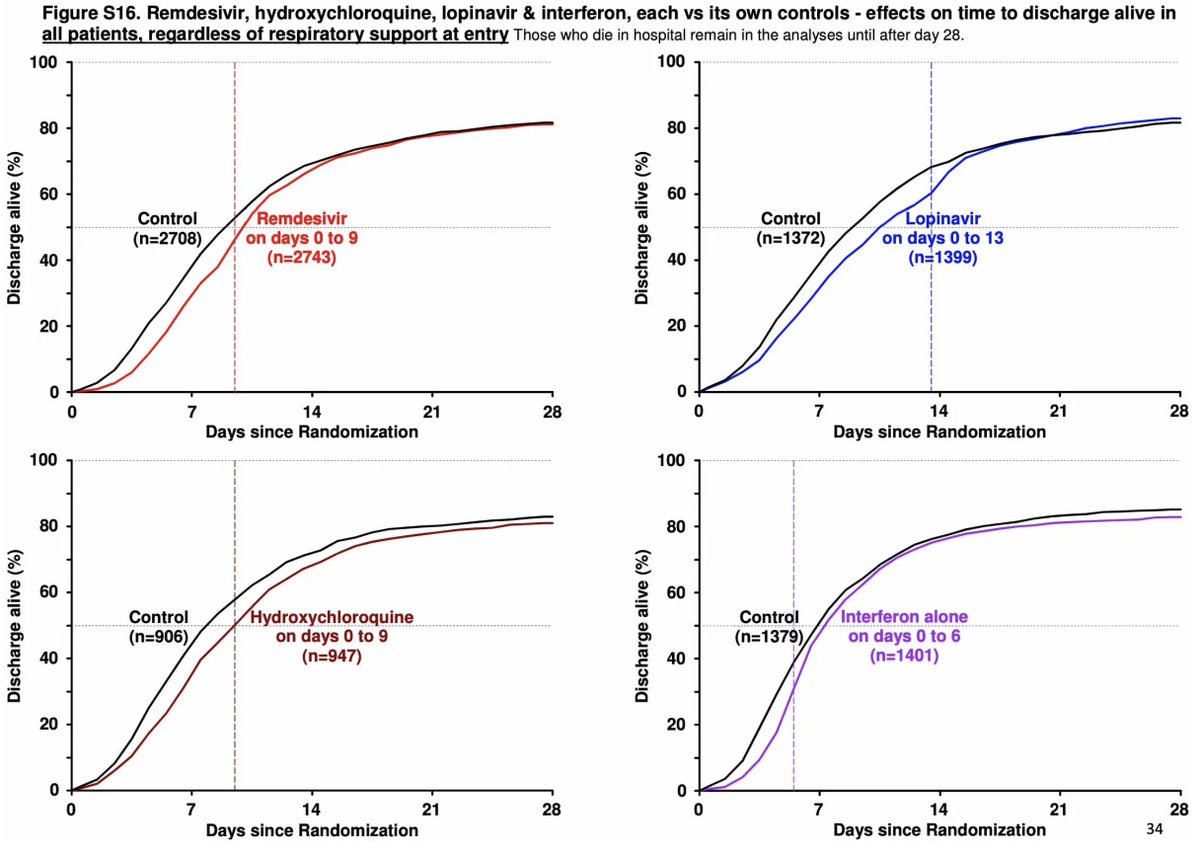
next: ACTT-1. blinded RCT of remdesivir found accelerated recovery in patients on remdesivir (without any effect on mortality). this became the raison d'etre of remdesivir - it would shorten hospitalization! woohoo! resources saved! 😀 (bit.ly/3AG8rH7) 

weird interlude: an RCT comparing 5 days vs. 10 days of remdesivir found no benefit from longer therapy, but maybe increased toxicity. whoops! keep on moving folks, there's nothing to see here!! 🤒 (bit.ly/3tWWqKv) 



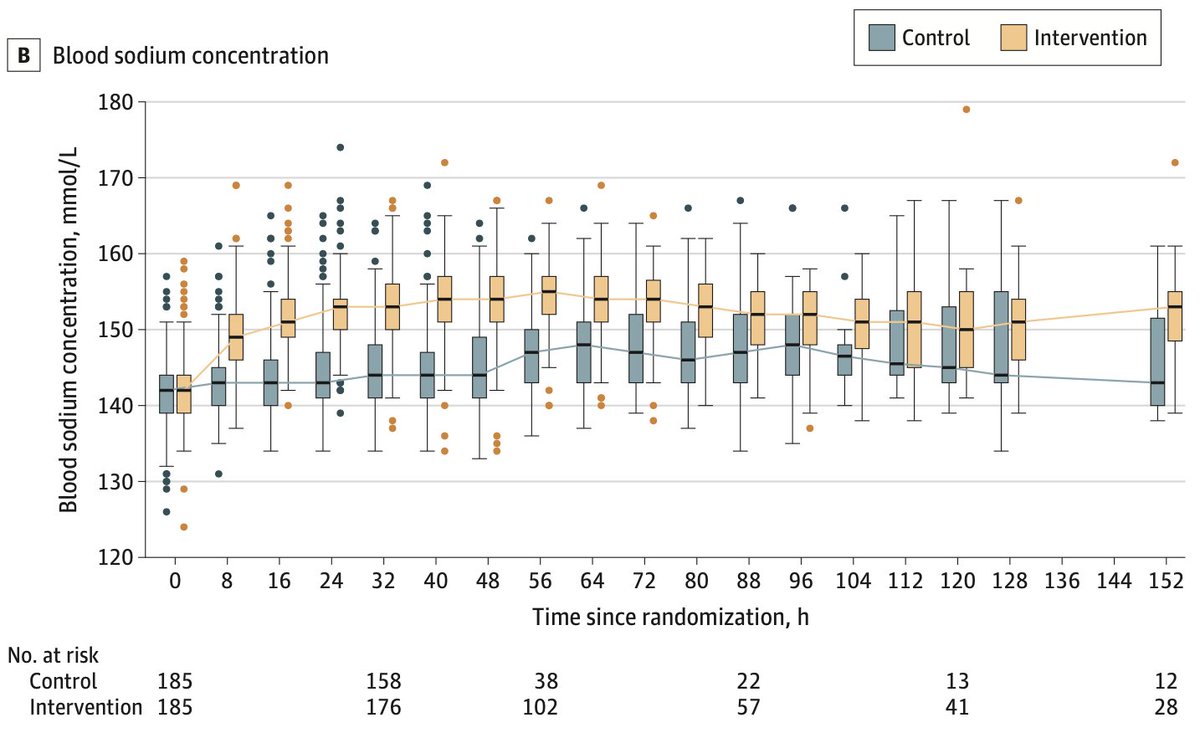
SOLIDARITY trial: when using the drug in an *open-label* fashion, patients treated with remdesivir actually spent *longer* in hospital (to finish their course). so the concept of using remdesivir to reduce hospital LOS & save resources is debunked 😩 (bit.ly/2Z72WmC) 


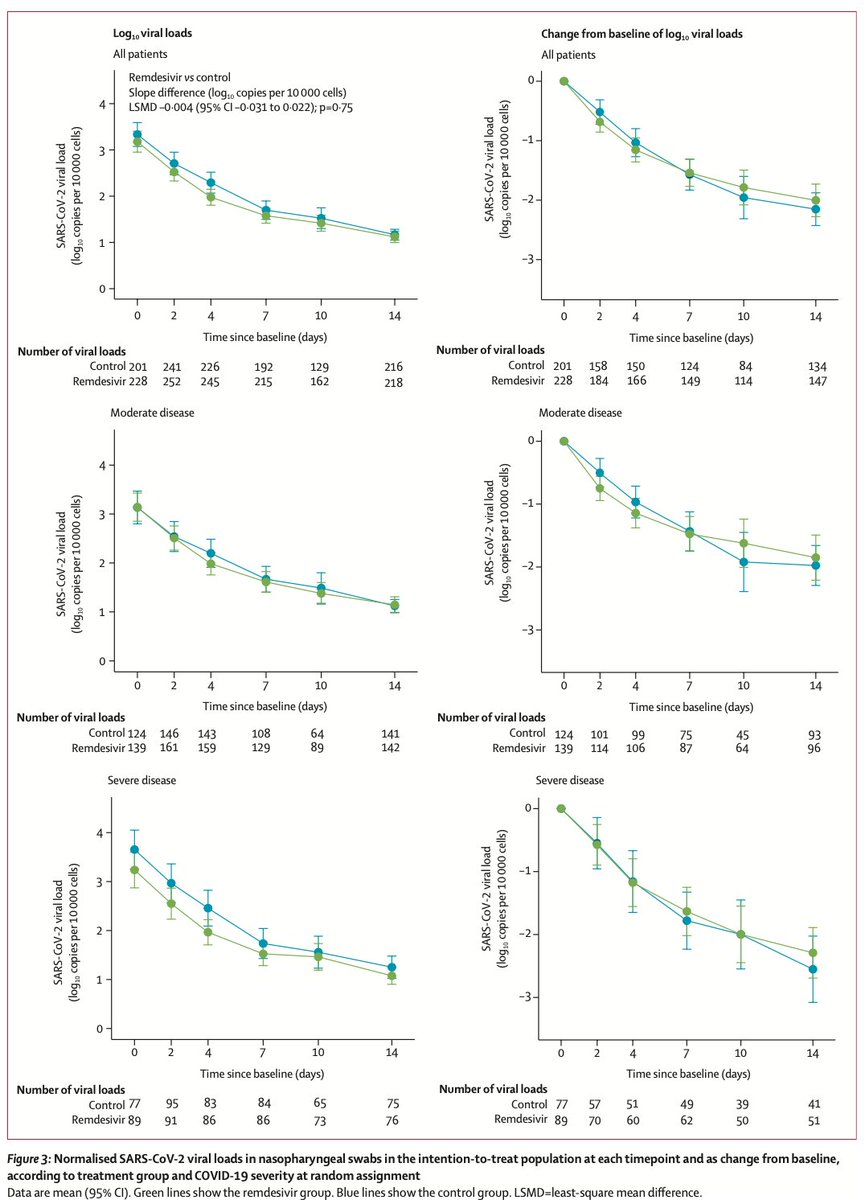
DISCOVERY trial: another open-label multicenter RCT that essentially replicates SOLIDARITY. no differences were found in clinical endpoints, mortality, viral load, or ventilator-free days. 😢 






this editorial on the DISCOVERY trial is a wee bit generous, but I agree with the conclusion - remdesivir administration should be restricted to clinical trials (until unequivocal benefit can be established) 🙏 



there is a threat that the goal posts on remdesivir could be shifted once again, based on a weird secondary composite endpoint. please note that this would be the THIRD shift:↔️
1) remdesivir saves lives
2) remdesivir saves hospital beds
3) remdesivir affects weird composite
1) remdesivir saves lives
2) remdesivir saves hospital beds
3) remdesivir affects weird composite

key point from the fine print: pregnant or potentially pregnant women were excluded in these trials (including ACTT-1; shame on NEJM for sneaking this into the supplemental). remdesivir is a nucleotide analog with potential teratogenicity - so its use in pregnancy is sketchy 😬 



so where does this leave us? remdesivir is basically the NIH's version of hydroxychloroquine or ivermectin. it doesn't work, but it's nearly impossible to stomp out. as quickly as it is proven to fail for one thing, the goal posts immediately shift to another target 🪳
the reason remdesivir fails to work in most hospitalized patients is that viral load is *already* dropping by the time patients get very sick. so immunomodulators work, but antivirals don't 🤷♂️ (bit.ly/3nQThLf) 



• • •
Missing some Tweet in this thread? You can try to
force a refresh