1/🧵
Did you know that heparin can cause hyperkalemia?
But why would an anticoagulant like heparin increase serum K⁺ levels?
The answer also has a wild implication - that heparin may itself have a diuretic effect...
#medtwitter #tweetorial
Did you know that heparin can cause hyperkalemia?
But why would an anticoagulant like heparin increase serum K⁺ levels?
The answer also has a wild implication - that heparin may itself have a diuretic effect...
#medtwitter #tweetorial

2/
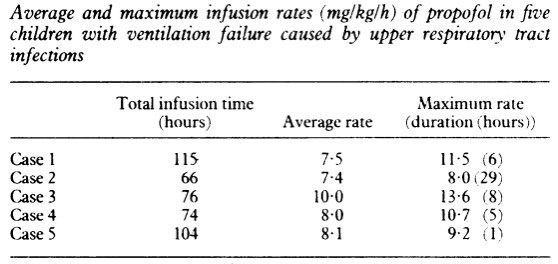
The first report of heparin-associated hyperkalemia occurred in 1964.
A patient had extended heparin exposure and developed progressive hyperkalemia (peak K⁺ level was 6.4 mEq/L), without another explanation.
pubmed.ncbi.nlm.nih.gov/14142415/
The first report of heparin-associated hyperkalemia occurred in 1964.
A patient had extended heparin exposure and developed progressive hyperkalemia (peak K⁺ level was 6.4 mEq/L), without another explanation.
pubmed.ncbi.nlm.nih.gov/14142415/

3/
Multiple subsequent case series reported hyperkalemia after heparin exposure.
💡While the exact incidence of heparin-associated hyperkalemia is unknown, it has been estimated at about 7%.
pubmed.ncbi.nlm.nih.gov/7778574/
Multiple subsequent case series reported hyperkalemia after heparin exposure.
💡While the exact incidence of heparin-associated hyperkalemia is unknown, it has been estimated at about 7%.
pubmed.ncbi.nlm.nih.gov/7778574/
4/
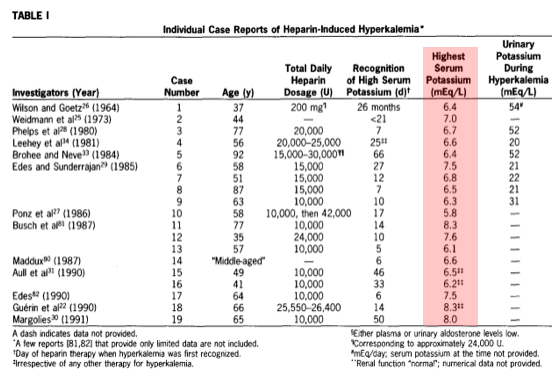
Similar results were also seen after low molecular weight heparin exposure, with potassium levels rising within 3 days.
9% of patients had potassium levels greater than 5 mEq/L.
ncbi.nlm.nih.gov/pmc/articles/P…
Similar results were also seen after low molecular weight heparin exposure, with potassium levels rising within 3 days.
9% of patients had potassium levels greater than 5 mEq/L.
ncbi.nlm.nih.gov/pmc/articles/P…
5/
So why can heparin exposure induce (usually mild) hyperkalemia?
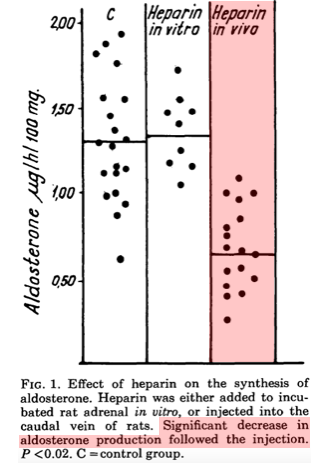
🔑It turns out that heparin reliably reduces adrenal aldosterone production, as observed in rats in the 1960s.
Heparin significantly reduced the rats' serum aldosterone levels.
pubmed.ncbi.nlm.nih.gov/14122519/
So why can heparin exposure induce (usually mild) hyperkalemia?
🔑It turns out that heparin reliably reduces adrenal aldosterone production, as observed in rats in the 1960s.
Heparin significantly reduced the rats' serum aldosterone levels.
pubmed.ncbi.nlm.nih.gov/14122519/
6/
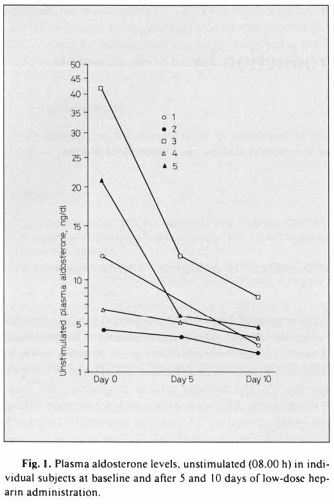
Studies in humans have confirmed the same association.
💥Treatment with heparin, even at prophylactic doses, results in reduction in serum aldosterone levels.
pubmed.ncbi.nlm.nih.gov/3740124/
Studies in humans have confirmed the same association.
💥Treatment with heparin, even at prophylactic doses, results in reduction in serum aldosterone levels.
pubmed.ncbi.nlm.nih.gov/3740124/
7/
Heparin is so good at blocking aldosterone secretion, it can suppress aldosterone production even w/ HYPERaldosteronism.
In the below case, a heparin analog totally suppressed aldosterone in a patient w/ a hyperfunctional adrenal adenoma.
pubmed.ncbi.nlm.nih.gov/4222823/
Heparin is so good at blocking aldosterone secretion, it can suppress aldosterone production even w/ HYPERaldosteronism.
In the below case, a heparin analog totally suppressed aldosterone in a patient w/ a hyperfunctional adrenal adenoma.
pubmed.ncbi.nlm.nih.gov/4222823/

8/
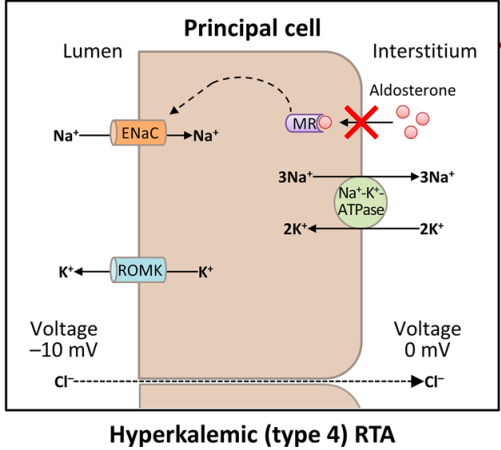
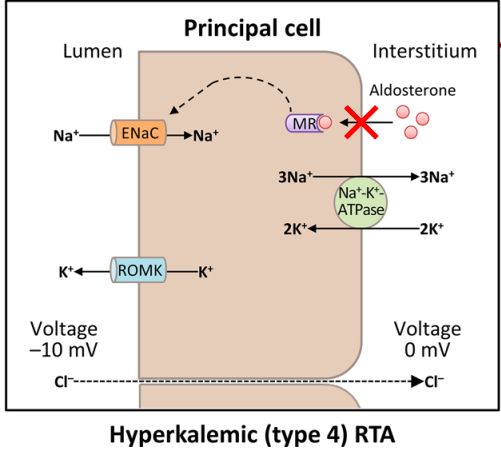
Why would blocking aldosterone production lead to hyperkalemia?
Recall that aldosterone mediates distal nephron K⁺ excretion via activation of the Na⁺-K⁺ ATPase and ENaC channel.
⬇️ aldosterone levels causes a hyperkalemic type IV RTA.
pubmed.ncbi.nlm.nih.gov/33367987/
Why would blocking aldosterone production lead to hyperkalemia?
Recall that aldosterone mediates distal nephron K⁺ excretion via activation of the Na⁺-K⁺ ATPase and ENaC channel.
⬇️ aldosterone levels causes a hyperkalemic type IV RTA.
pubmed.ncbi.nlm.nih.gov/33367987/
9/
We have established that heparin can cause hyperkalemia via decreased aldosterone production.
But we're still left with the question, how does heparin mediate this effect?
We have established that heparin can cause hyperkalemia via decreased aldosterone production.
But we're still left with the question, how does heparin mediate this effect?
10/
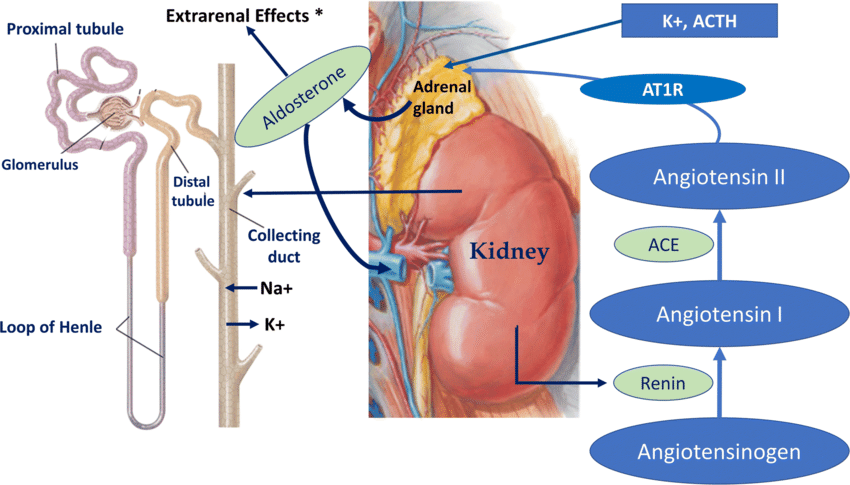
Aldosterone production from the adrenal gland's zona glomerulosa is stimulated primarily by angiotensin II (in addition to ACTH), as part of the Renin-Angiotensin-Aldosterone system.
pubmed.ncbi.nlm.nih.gov/30826898/
Aldosterone production from the adrenal gland's zona glomerulosa is stimulated primarily by angiotensin II (in addition to ACTH), as part of the Renin-Angiotensin-Aldosterone system.
pubmed.ncbi.nlm.nih.gov/30826898/
11/
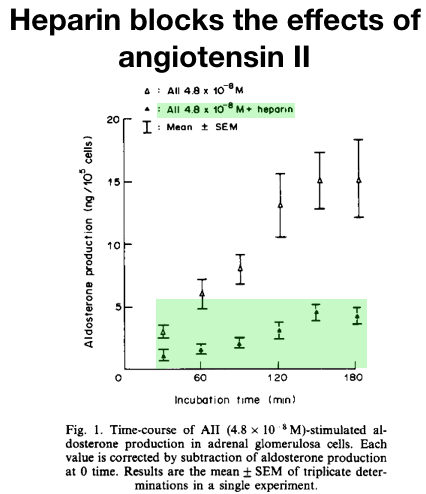
🔑It turns out that heparin blocks the effects of angiotensin II.
As can be seen from this study in rat zona glomerulosa cells, heparin blocks angiotensin-mediated aldosterone secretion.
pubmed.ncbi.nlm.nih.gov/3022074/
🔑It turns out that heparin blocks the effects of angiotensin II.
As can be seen from this study in rat zona glomerulosa cells, heparin blocks angiotensin-mediated aldosterone secretion.
pubmed.ncbi.nlm.nih.gov/3022074/
12/
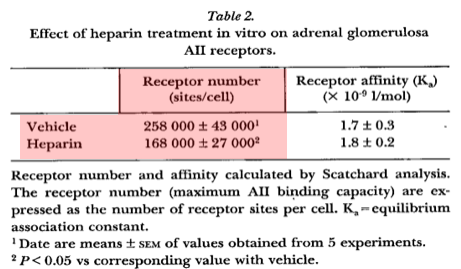
There is at least 1, and possibly 2, reasons for why heparin blocks angiotensin-induced aldosterone production.
💡First, heparin directly decreases angiotensin II receptor expression on adrenal zona glomerulosa cells (in rats, at least).
pubmed.ncbi.nlm.nih.gov/3188809/
There is at least 1, and possibly 2, reasons for why heparin blocks angiotensin-induced aldosterone production.
💡First, heparin directly decreases angiotensin II receptor expression on adrenal zona glomerulosa cells (in rats, at least).
pubmed.ncbi.nlm.nih.gov/3188809/
13/
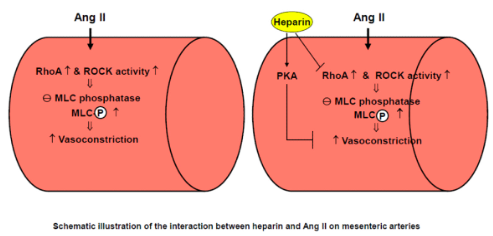
💡Heparin also blocks angiotensin II-mediated intracellular signaling within vascular endothelial cells.
Whether heparin has the same effect on adrenal zona glomerulosa cells is unknown.
ncbi.nlm.nih.gov/pmc/articles/P…
💡Heparin also blocks angiotensin II-mediated intracellular signaling within vascular endothelial cells.
Whether heparin has the same effect on adrenal zona glomerulosa cells is unknown.
ncbi.nlm.nih.gov/pmc/articles/P…
14/
Let's end with a fascinating wrinkle that really surprised me.
We established that heparin causes hyperkalemia by blocking angiotensin's stimulation of aldosterone production.
⬇️ aldosterone should also lead to ⬆️ sodium excretion (similar to K⁺ sparing diuretics).
Let's end with a fascinating wrinkle that really surprised me.
We established that heparin causes hyperkalemia by blocking angiotensin's stimulation of aldosterone production.
⬇️ aldosterone should also lead to ⬆️ sodium excretion (similar to K⁺ sparing diuretics).
15/
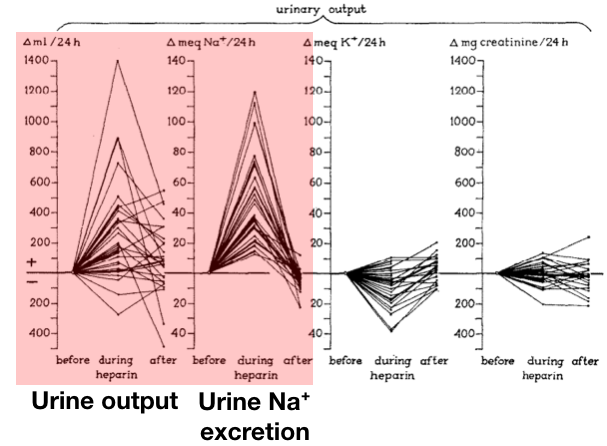
💥This implies that when heparin blocks aldosterone production, it may indirectly act as a diuretic.
A clinical case series from 1960 suggested that this can occur.
💥This implies that when heparin blocks aldosterone production, it may indirectly act as a diuretic.
A clinical case series from 1960 suggested that this can occur.
16/
The authors treated 29 hypervolemic patients with heparin (w/the goal of achieving diuresis).
🔑They found that heparin often did lead to diuresis, w/ increased urinary sodium excretion and urine output.
pubmed.ncbi.nlm.nih.gov/14420094/
The authors treated 29 hypervolemic patients with heparin (w/the goal of achieving diuresis).
🔑They found that heparin often did lead to diuresis, w/ increased urinary sodium excretion and urine output.
pubmed.ncbi.nlm.nih.gov/14420094/
17/
They also noted clinical responses, including significant reduction of body weight and peripheral edema.
In the case below, extended heparin treatment led to an 8 kg diuresis in a patient with nephrotic syndrome.
pubmed.ncbi.nlm.nih.gov/14420094/
They also noted clinical responses, including significant reduction of body weight and peripheral edema.
In the case below, extended heparin treatment led to an 8 kg diuresis in a patient with nephrotic syndrome.
pubmed.ncbi.nlm.nih.gov/14420094/

18/
Heparin seems to have potential diuretic effects through its ability to inhibit aldosterone production.
But the arrival of more effective and safe diuretics in the 1960s (eg furosemide) likely explains why additional studies of this potential drug effect never occurred.
Heparin seems to have potential diuretic effects through its ability to inhibit aldosterone production.
But the arrival of more effective and safe diuretics in the 1960s (eg furosemide) likely explains why additional studies of this potential drug effect never occurred.
19/SUMMARY
🍌 Heparin can cause hyperkalemia by ⬇️ aldosterone production
🍌 This occurs b/c heparin ⬇️ adrenal angiotensin II receptor expression, and possibly inhibition of intracellular signaling
🍌 Heparin may also have indirect diuretic effects as a result of ⬇️ aldosterone
🍌 Heparin can cause hyperkalemia by ⬇️ aldosterone production
🍌 This occurs b/c heparin ⬇️ adrenal angiotensin II receptor expression, and possibly inhibition of intracellular signaling
🍌 Heparin may also have indirect diuretic effects as a result of ⬇️ aldosterone
• • •
Missing some Tweet in this thread? You can try to
force a refresh