1/ Our article on historical droplet error (#DropletDogma) just published after peer-review
"How did we get here: what are droplets and aerosols and how far do they go? A historical perspective on the transmission of respiratory infectious diseases"
doi.org/10.1098/rsfs.2…
"How did we get here: what are droplets and aerosols and how far do they go? A historical perspective on the transmission of respiratory infectious diseases"
doi.org/10.1098/rsfs.2…
2/ An honor to have worked in an interdisciplinary team led by @linseymarr and Lydia Bourouiba of @MIT, together with the amazing @katierandall and @EThomasEwing
TL;DR: understanding of "droplets" in medicine is based on large errors that went mostly unnoticed until now
TL;DR: understanding of "droplets" in medicine is based on large errors that went mostly unnoticed until now
3/ We have written a review article on the wider arc of history, which is now under peer-review, preprint here:
papers.ssrn.com/sol3/papers.cf…
Already ranked #1 on their Infectious Diseases e-journal: papers.ssrn.com/sol3/topten/to…
papers.ssrn.com/sol3/papers.cf…
Already ranked #1 on their Infectious Diseases e-journal: papers.ssrn.com/sol3/topten/to…
4/ That last paper is based on this thread on the history of airborne transmission which I wrote last summer.
https://twitter.com/jljcolorado/status/1391111720526024708
5/ Back to the just published paper by @katierandall et al. What did we learn?
History over last century conditioned the evolution of the field of infectious disease transmission, leading to a couple of errors becoming entrenched into the #DropletDogma, and denial of airborne
History over last century conditioned the evolution of the field of infectious disease transmission, leading to a couple of errors becoming entrenched into the #DropletDogma, and denial of airborne

6/ Historically it was thought that diseases transmitted through the air, often over long distances and in a phantasmagorical way, and miasma theory was dominant.
en.wikipedia.org/wiki/Miasma_th…
en.wikipedia.org/wiki/Miasma_th…

7/ As we explain on preprint & history thread, that starts to change in 2nd half of the 19th century: cholera, purpural fever, malaria were thought to be transmitted through the air, but we learn that are REALLY transmitted by water, hands, mosquitoes.
https://twitter.com/jljcolorado/status/1391121403584434180
8/ Germ theory changes the paradigm of transmission, and miasma theory is vanquished.
However for many diseases the modes of transmission are still unclear. People still think many diseases go through the air.
However for many diseases the modes of transmission are still unclear. People still think many diseases go through the air.
9/ Charles Chapin is a prominent American epidemiologist (en.wikipedia.org/wiki/Charles_V…). Operating only a few decades after the huge paradigm shift of germ theory, he is trying to establish "contact infection" as the most important 

10/ C. encounters much resistance to views on importance of contact infection. Writes in seminal 1910 book (google.com/books/edition/…):
"I have sometimes been told I lay too much emphasis on contact infection,” although "until recently very little attention has been paid to it"
"I have sometimes been told I lay too much emphasis on contact infection,” although "until recently very little attention has been paid to it"
11/ A key reason why there is resistance is bc people still think that transmission is through the air.
“It is impossible to teach people to avoid contact infection while they are firmly convinced that the air is the chief vehicle of infection” (archive.org/details/source…)
“It is impossible to teach people to avoid contact infection while they are firmly convinced that the air is the chief vehicle of infection” (archive.org/details/source…)

12/ Chapin acknowledges that there is no evidence to rule out airborne transmission, as methods were too primitive:
“In air infection, it becomes evident that our knowledge is far too scanty, and that the available evidence is far from conclusive”
archive.org/details/source…
“In air infection, it becomes evident that our knowledge is far too scanty, and that the available evidence is far from conclusive”
archive.org/details/source…
13/ But nevertheless, Chapin proceeds to interpret ease of infection in close proximity as due to "spray-borne droplets" and NOT short-range airborne transmission.
(The SAME error still being made by @WHO and most ID researchers, comes from Chapin!!)
archive.org/details/source…
(The SAME error still being made by @WHO and most ID researchers, comes from Chapin!!)
archive.org/details/source…

14/ And in an attempt to establish the importance of contact infection, C turns absence of evidence in favor of airborne into evidence of absence:
“There is no evidence that [air infection] is an appreciable factor in the maintenance of most of our common contagious diseases."
“There is no evidence that [air infection] is an appreciable factor in the maintenance of most of our common contagious diseases."
15/ [Continued]
"We are warranted, then, in discarding it as a working hypothesis, and devoting our chief attention to the prevention of contact infection.”
"We are warranted, then, in discarding it as a working hypothesis, and devoting our chief attention to the prevention of contact infection.”

16/ This is the key error. Chapin is too successful in changing paradigm while trying to kill off the miasma remains, & to establish his theory of contact infection
#DropletDogma established:
- Ease of infection in proximity --> evidence of droplets
- Airborne almost impossible
#DropletDogma established:
- Ease of infection in proximity --> evidence of droplets
- Airborne almost impossible
17/ Curiously, many people refer to spray-borne droplets as "Flugge's droplets." This is another error.
Lydia B. read the original works of Flugge. They used "droplet" to refer to both droplets and aerosols, and WAITED 5 HOURS for aerosols to settle on their collection plates!
Lydia B. read the original works of Flugge. They used "droplet" to refer to both droplets and aerosols, and WAITED 5 HOURS for aerosols to settle on their collection plates!
18/ For example this prominent Spanish doctor is telling us that Flugge's droplets, which (according to him) are the main transmission mechanism of COVID, can be seen as impacted on your computer monitor if you turn it off.
Not what Flugge said!!
Not what Flugge said!!
https://twitter.com/DrLejarazu/status/1304689399226081281
19/ Some people may question how an epidemiologist who wrote a book in 1910 could be so influential to this day.
But the key is that Chapin's paradigm was widely accepted, and became the dogma in infectious disease transmission.
But the key is that Chapin's paradigm was widely accepted, and became the dogma in infectious disease transmission.
19/ For example, Alexander Langmuir, the first and longtime director of the epidemiology branch of @CDCgov, referred to Chapin in 1967 as in 1967 as "the greatest American epidemiologist"
"As late as the 1980s Chapin’s views were dominant [at @CDCgov"
academic.oup.com/aje/article/14…
"As late as the 1980s Chapin’s views were dominant [at @CDCgov"
academic.oup.com/aje/article/14…
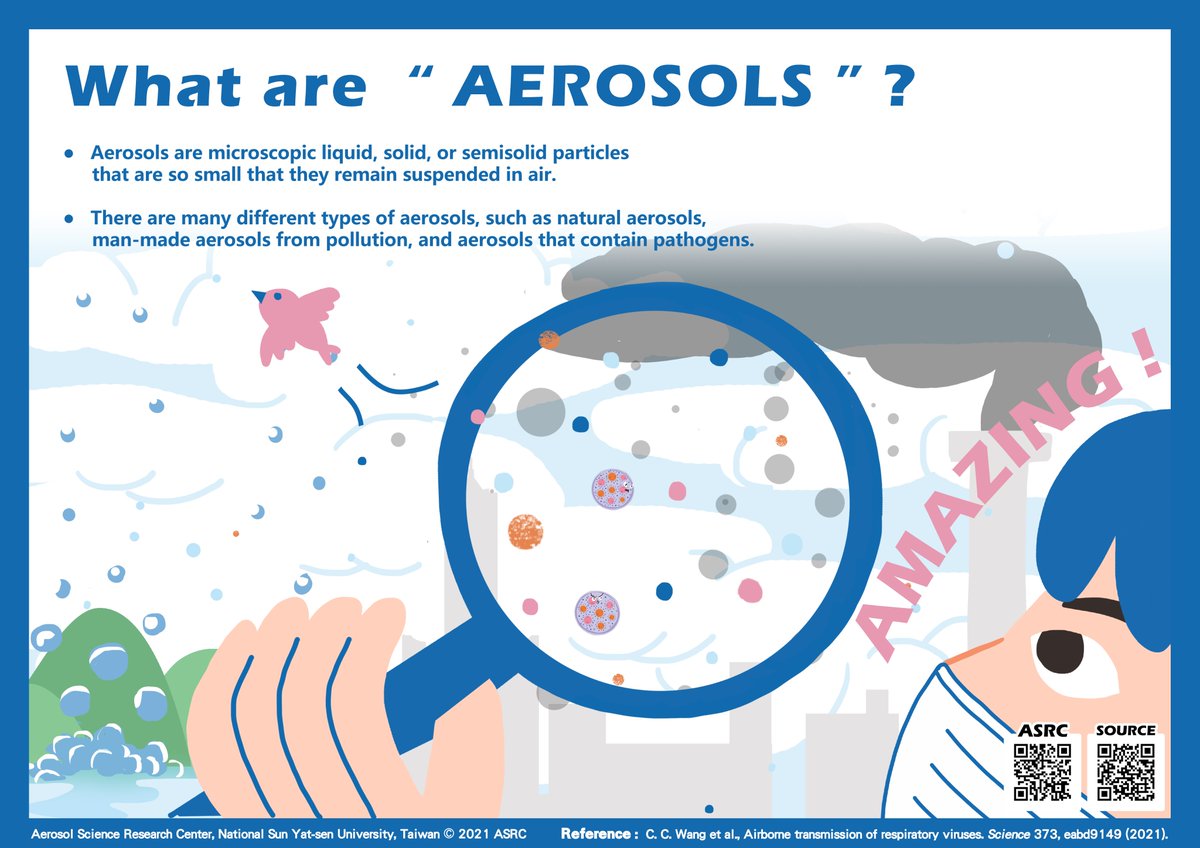
20/ Chapin's ideas were so dominant, that they lead to systematic misinterpretation of scientific results by Langmuir (en.wikipedia.org/wiki/Alexander…) et al.:
The assumed that increasing distance would reduce droplet infection, but NOT airborne infection!
academic.oup.com/aje/article/14…
The assumed that increasing distance would reduce droplet infection, but NOT airborne infection!
academic.oup.com/aje/article/14…

Langmuir's hypothesis: "If droplet spread were important, then double bunking, with more space between bunks, should decrease close contact, and illness should decrease. However, if spread were airborne, there should be no change in the illness rate"
academic.oup.com/aje/article/14…
academic.oup.com/aje/article/14…
This is an astounding error. Of course airborne transmission is more efficient in close proximity too, because infectious aerosols are far more concentrated there than in well-mixed room air!
Graphic by Prof. @linseymarr, published in journalofhospitalinfection.com/article/S0195-…
Graphic by Prof. @linseymarr, published in journalofhospitalinfection.com/article/S0195-…
23/ By the 1930s, Harvard engineering professor William Wells was applying more modern methods to airborne disease transmission. He thought that tuberculosis and measles were airborne. 

24/ But...
"Some rejected airborne trans. bc it ‘revived the ancient theory of miasmas’. [The Wellses] recognized the perception that a airborne transmission could be viewed as regressive, re-embracing obsolete ideas of ‘bad air’
royalsocietypublishing.org/doi/10.1098/rs…
"Some rejected airborne trans. bc it ‘revived the ancient theory of miasmas’. [The Wellses] recognized the perception that a airborne transmission could be viewed as regressive, re-embracing obsolete ideas of ‘bad air’
royalsocietypublishing.org/doi/10.1098/rs…
25/ In 1951, Langmuir (then head of epidemiology at @CDCgov) noted that "It remains to be proved that airborne infection is an important mode of spread of naturally occurring disease"
royalsocietypublishing.org/doi/10.1098/rs…
royalsocietypublishing.org/doi/10.1098/rs…
26/ It was only in 1962 that pulmonary tuberculosis, after 50 years of being described as a droplet disease, was finally shown by Wells, Riley et al. to be airborne (pubmed.ncbi.nlm.nih.gov/14492300/).
Today we know it is ONLY airborne.
Today we know it is ONLY airborne.

27/ Langmuir is interested on airborne transmission bc he has concluded that biological weapons can have airborne trans.
He learns from Wells that droplets smaller than 5 microns (um) can reach the deep lung. And < 5 um needed to transmit tuberculosis, bc need to reach alveoli
He learns from Wells that droplets smaller than 5 microns (um) can reach the deep lung. And < 5 um needed to transmit tuberculosis, bc need to reach alveoli
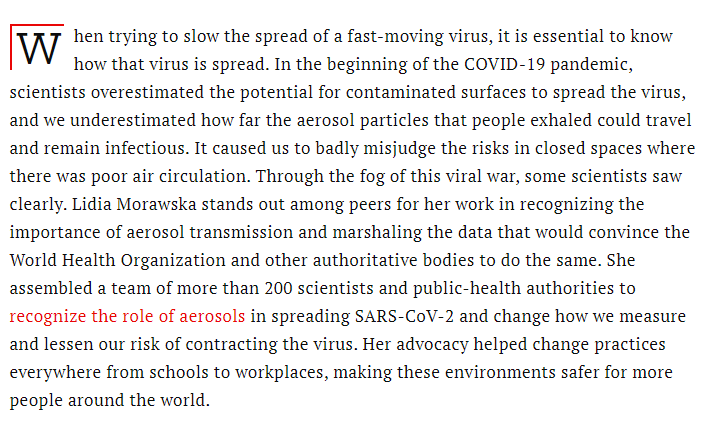
28/ It is around that time that the 5 um error crops up at @CDCgov. Someone confuses the size to reach the deep lung (< 5 um) with the size to fall to ground in 1-2 m from the person (> 100 um).
Error keeps being repeated, including by @WHO to this day.
Error keeps being repeated, including by @WHO to this day.

29/ @katierandall dogged research found the cause of the 5 um error (just described). We tried to trace references of 5 um and 1-2 um, they led nowhere
NO BASIS ANYWHERE IN SCI. LIT. for 5 micron = large droplets!! Yet @WHO repeats it without citation!
royalsocietypublishing.org/doi/10.1098/rs…
NO BASIS ANYWHERE IN SCI. LIT. for 5 micron = large droplets!! Yet @WHO repeats it without citation!
royalsocietypublishing.org/doi/10.1098/rs…

30/ This great article by @MeganMolteni in @wired tells the story of finding the 5 um error. I highly recommend it, it reads like a detective story:
wired.com/story/the-teen…
wired.com/story/the-teen…
31/ Yet, here we are, and @WHO and @CDCgov have acknowledge airborne transmission of COVID, but very confusingly, and without saying it clearly, making any announcements, and clearly putting forward the needed measures, as @zeynep summarizes here:
nytimes.com/2021/05/07/opi…
nytimes.com/2021/05/07/opi…
32/ People are dying every day because of this stubborn refusal by many in public health and infectious diseases to accept the overwhelming evidence that COVID-19 is a predominantly airborne disease (as we published months ago in @TheLancet).
https://twitter.com/jljcolorado/status/1383566908797059078
33/ If you find the history interesting and want more details, the two papers and previous thread have lots of it:
- royalsocietypublishing.org/doi/10.1098/rs…
- papers.ssrn.com/sol3/papers.cf…
-
- royalsocietypublishing.org/doi/10.1098/rs…
- papers.ssrn.com/sol3/papers.cf…
-
https://twitter.com/jljcolorado/status/1391111720526024708
34/ And I recently gave an @isiaq webinar on this history of airborne transmission, which can be watched in YouTube at:
(The prior talk by Lidia Morawska in the same webinar is pure gold)
(The prior talk by Lidia Morawska in the same webinar is pure gold)
35/ As always more than happy to receive feedback, including anything anyone thinks is inaccurate, erroneous etc.
#COVIDisAirborne
#COVIDisAirborne
• • •
Missing some Tweet in this thread? You can try to
force a refresh