
1/
A #tweetorial about simulation in NCC
Today @namorris opened his remarks on Sim in NCC @ #NCS2021 w/ a simple question about the correct first line treatment for SE? Everyone got it.
Then he posed a tougher question.
How often does that happen?
No one voted "always"
A #tweetorial about simulation in NCC
Today @namorris opened his remarks on Sim in NCC @ #NCS2021 w/ a simple question about the correct first line treatment for SE? Everyone got it.
Then he posed a tougher question.
How often does that happen?
No one voted "always"
2/
Even the most groundbreaking research won’t benefit our patients if we aren’t delivering it correctly.
I so highly encourage you to check out Nick’s talk on-demand if you have access to #NCS2021.
It is 🚨critical🚨 that we teach more effectively!
Even the most groundbreaking research won’t benefit our patients if we aren’t delivering it correctly.
I so highly encourage you to check out Nick’s talk on-demand if you have access to #NCS2021.
It is 🚨critical🚨 that we teach more effectively!
4/
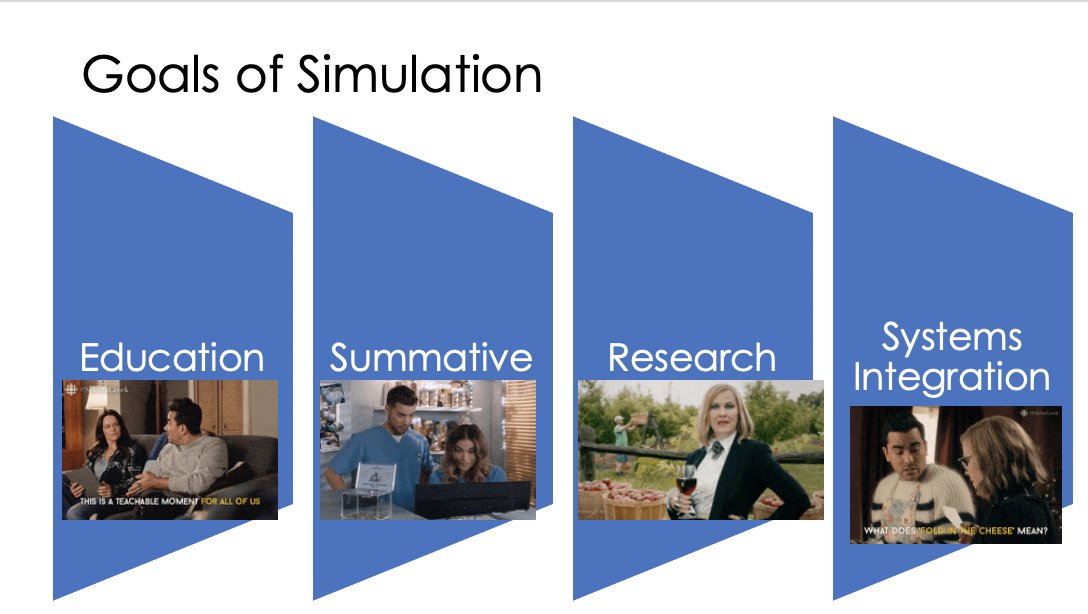
Simulation is an amazing educational tool. But it can be used in other ways, too!
Simulation can be used to:
⭐️to evaluate trainees
⚡️ as a research tool to understand learners and systems
✨to understanding systems integration & improve care delivery.
Simulation is an amazing educational tool. But it can be used in other ways, too!
Simulation can be used to:
⭐️to evaluate trainees
⚡️ as a research tool to understand learners and systems
✨to understanding systems integration & improve care delivery.
5/
Defining the simulation’s goal is defining the “Why”.
And if you are interested in approaching this as research, it is crucial to approach it with a hypothesis and have a methodology in mind from the start. Another amazing pearl from @namorris.
Defining the simulation’s goal is defining the “Why”.
And if you are interested in approaching this as research, it is crucial to approach it with a hypothesis and have a methodology in mind from the start. Another amazing pearl from @namorris.
6/
From the “why” you also will need to define the purpose of the sim -- the “what”:
“what is the learning object” “What are we trying to improve with this?”
Lots of options:
From the “why” you also will need to define the purpose of the sim -- the “what”:
“what is the learning object” “What are we trying to improve with this?”
Lots of options:

7/
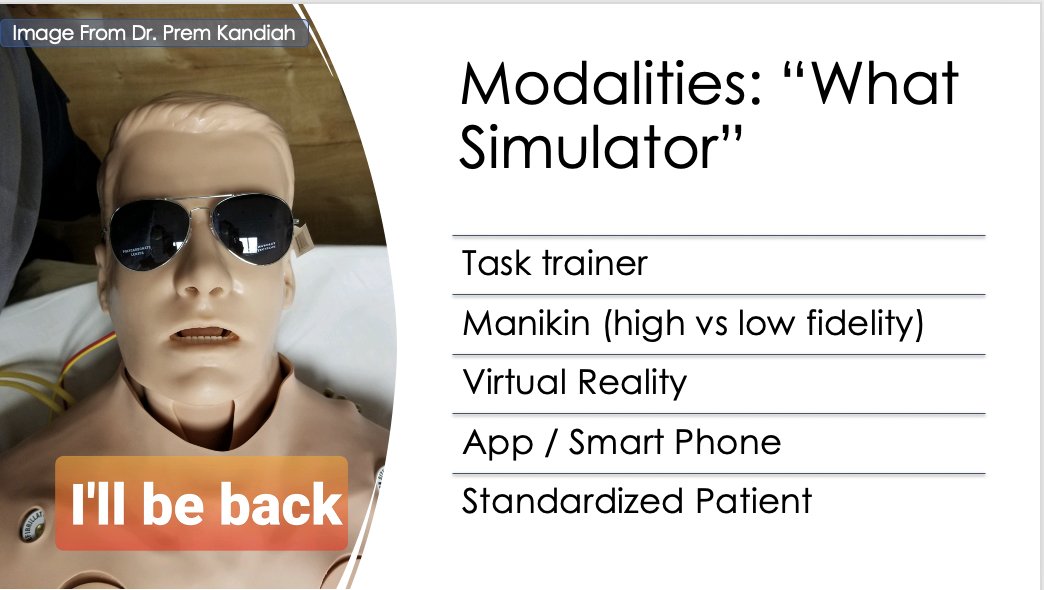
What you want to accomplish defines “how” you should accomplish this. Simulation can be done through tissue models, task trainers, manikins, apps, virtual reality, standardized patient, and more
What you want to accomplish defines “how” you should accomplish this. Simulation can be done through tissue models, task trainers, manikins, apps, virtual reality, standardized patient, and more
8/
It seems straight forward but the fidelity is only “high” or “low” in reference to your goal --
👉Teaching LPs on a task trainer is “high fidelity”
👉Teaching communication and leadership training with a task trainer…
It seems straight forward but the fidelity is only “high” or “low” in reference to your goal --
👉Teaching LPs on a task trainer is “high fidelity”
👉Teaching communication and leadership training with a task trainer…
9/
So we’ve got the “Why do this” & “What is the purpose” & “How are we going to do this”
But u also need “How are we going to run the case?”
A tradition model is to run the case & debrief @ the end
But, as @Capt_Ammonia loves, you can also rapid cycle & debrief as you go!
So we’ve got the “Why do this” & “What is the purpose” & “How are we going to do this”
But u also need “How are we going to run the case?”
A tradition model is to run the case & debrief @ the end
But, as @Capt_Ammonia loves, you can also rapid cycle & debrief as you go!
10/
Putting it all together. Each simulation:
👉has an overall goal: the “WHY” do this
👉has a purpose & specific learning objectives: the “WHAT” is it we are trying to accomplish
👉has a modality and method: the ”HOW” we are going to run the case
Putting it all together. Each simulation:
👉has an overall goal: the “WHY” do this
👉has a purpose & specific learning objectives: the “WHAT” is it we are trying to accomplish
👉has a modality and method: the ”HOW” we are going to run the case

10/
Some examples I love that have used simulation in neurology/neurocrit care:
pubmed.ncbi.nlm.nih.gov/33005731/
pubmed.ncbi.nlm.nih.gov/22675080/
pubmed.ncbi.nlm.nih.gov/29467974/
pubmed.ncbi.nlm.nih.gov/25898887/
pubmed.ncbi.nlm.nih.gov/32424536/
Some examples I love that have used simulation in neurology/neurocrit care:
pubmed.ncbi.nlm.nih.gov/33005731/
pubmed.ncbi.nlm.nih.gov/22675080/
pubmed.ncbi.nlm.nih.gov/29467974/
pubmed.ncbi.nlm.nih.gov/25898887/
pubmed.ncbi.nlm.nih.gov/32424536/
11/
But simulation in neurocritical care has its own challenges.
1⃣How real is real enough?
A manikin falls short in the neuro exam.
Want to learn what the Babinski sign looks like?... manikin isn't going to cut it.
Check out @grepmeded instead
But simulation in neurocritical care has its own challenges.
1⃣How real is real enough?
A manikin falls short in the neuro exam.
Want to learn what the Babinski sign looks like?... manikin isn't going to cut it.
Check out @grepmeded instead
12/
But in the context of stroke, seizure, brain death, etc if you want to train learners to initiate a diagnostic workup, interpret radiology, correctly dose medications, screen for confounders, communicate findings… The manikin’s exam matters less.
But in the context of stroke, seizure, brain death, etc if you want to train learners to initiate a diagnostic workup, interpret radiology, correctly dose medications, screen for confounders, communicate findings… The manikin’s exam matters less.
13/
Work Sahar Zafar & I did @ MGH Learning Lab demonstrating that residents gained the same amount of confidence and knowledge in simulations with SPs as they did with a manikin. So glad @DanHarrisonMD and others are carrying this work forward @harvardneuromds!
Work Sahar Zafar & I did @ MGH Learning Lab demonstrating that residents gained the same amount of confidence and knowledge in simulations with SPs as they did with a manikin. So glad @DanHarrisonMD and others are carrying this work forward @harvardneuromds!

14/
2⃣nd challenge: Does a learner’s performance in the sim lab correlate with how they are going to perform in real life?
This study (@namorris) suggests so! Sim-Based Assessment of Graduate Neurology Trainees' Performance Managing Acute Ischemic Stroke pubmed.ncbi.nlm.nih.gov/34706974/
2⃣nd challenge: Does a learner’s performance in the sim lab correlate with how they are going to perform in real life?
This study (@namorris) suggests so! Sim-Based Assessment of Graduate Neurology Trainees' Performance Managing Acute Ischemic Stroke pubmed.ncbi.nlm.nih.gov/34706974/
15/
Finally – how are we going to prove that the work we do in a simulation lab translates to what really matters: improving patient outcomes.
It can be done but it's a challenge and requires a lot of accounting for confounders... the opposite of:
Finally – how are we going to prove that the work we do in a simulation lab translates to what really matters: improving patient outcomes.
It can be done but it's a challenge and requires a lot of accounting for confounders... the opposite of:
15/
But, I'm confident we in neuro/NCC we can overcome these challenges; there are so many awesome educators passionate about improving the delivery of care through sim @Tracey1milligan @captammonia @ghoshal_shivani @judyhtchang @aartisarwal @drdangayach @namorrismd and others!!
But, I'm confident we in neuro/NCC we can overcome these challenges; there are so many awesome educators passionate about improving the delivery of care through sim @Tracey1milligan @captammonia @ghoshal_shivani @judyhtchang @aartisarwal @drdangayach @namorrismd and others!!
16/
I hope we can come together do multi-site studies and measure our impact!
And if you're new to sim, I cannot, cannot, cannot recommend the course at @MedSimulation more highly. Truly, it is LIFE CHANGING.
@GetCuriousNow @sim_podcast
I hope we can come together do multi-site studies and measure our impact!
And if you're new to sim, I cannot, cannot, cannot recommend the course at @MedSimulation more highly. Truly, it is LIFE CHANGING.
@GetCuriousNow @sim_podcast
17/
Thank you again, @namorris and @neurocritical for inviting me to speak. Its exciting to see #meded in #NCS2021! So excited for what the future of sim in neurocritical care!! #NCS2022
(And for fun sims @ @EmoryNeuroCrit! @JimmySuhMD @CajalButterfly @sigman_md @EricLawson90!)
Thank you again, @namorris and @neurocritical for inviting me to speak. Its exciting to see #meded in #NCS2021! So excited for what the future of sim in neurocritical care!! #NCS2022
(And for fun sims @ @EmoryNeuroCrit! @JimmySuhMD @CajalButterfly @sigman_md @EricLawson90!)
• • •
Missing some Tweet in this thread? You can try to
force a refresh









