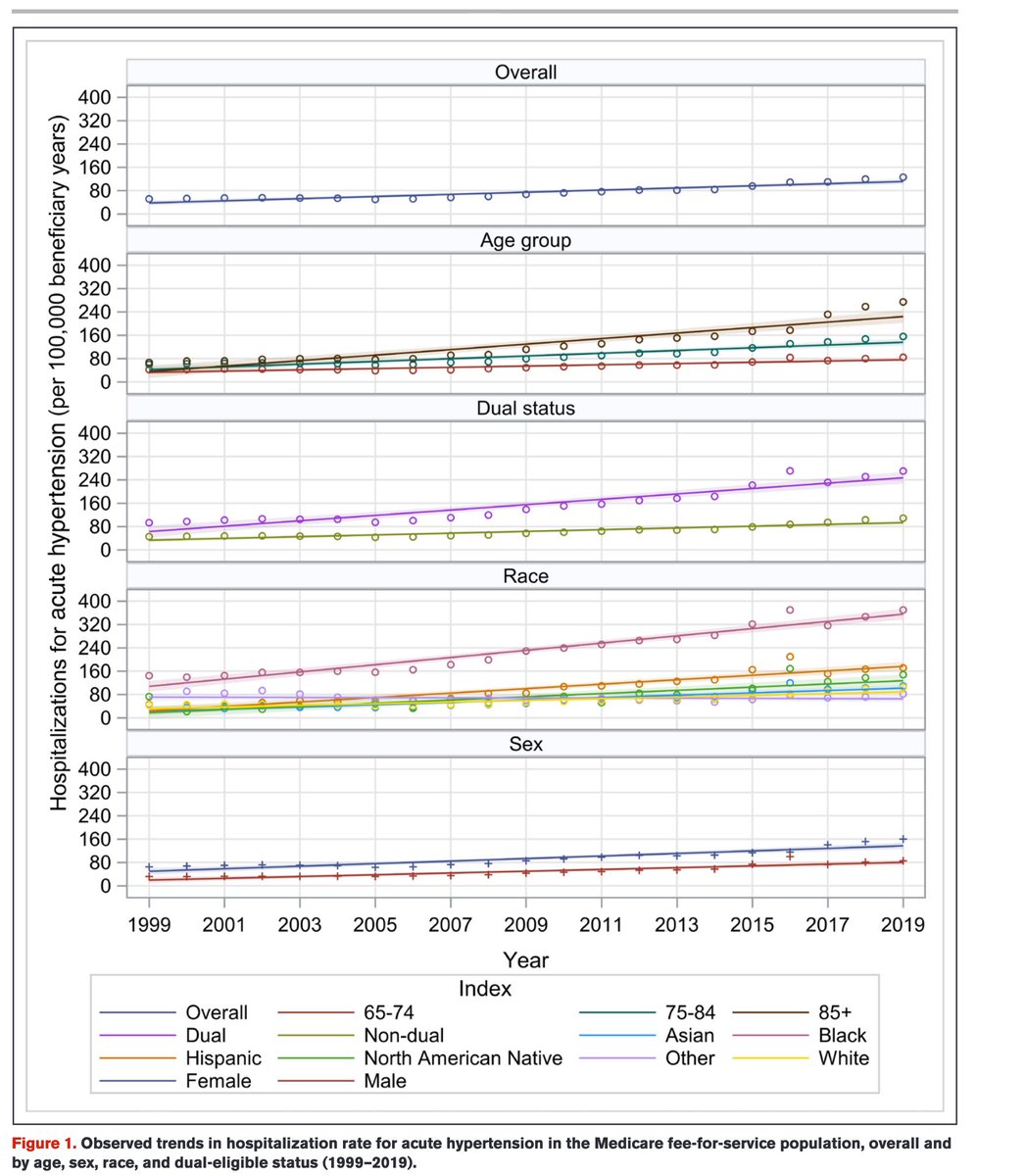
Resistant #hypertension is elevated BP despite the use of 3 antihypertensive drugs. We now introduce persistent hypertension, a broader concept of persistently elevated blood pressure. @amjmed amjmed.com/article/S0002-… @YaleMed @YaleCardiology #BloodPressure 
@amjmed @YaleMed @YaleCardiology Resistant hypertension focuses attention on those already treated with maximum doses; persistent hypertension is broader, those with persistently elevated blood pressure, for a wide range of reasons - and this is the vast majority who languish at high risk. @yuan_lu1 @amjmed 

@amjmed @YaleMed @YaleCardiology @yuan_lu1 To make progress against hypertension we need to focus intently on those with persistent hypertension; high bp readings over time, without progress. There are so many reasons; and many are social in nature. And this burden falls hard on Black patients in particular.
@amjmed @YaleMed @YaleCardiology @yuan_lu1 There are many causes of persistent hypertension; they represent targets for our strategies to help our patients lower risk. The Figure shows issues, barriers, & potential actions. Hypertension control is not just about writing prescriptions. amjmed.com/article/S0002-… @DrTomFrieden 

@amjmed @YaleMed @YaleCardiology @yuan_lu1 @DrTomFrieden "a broader concept of persistent hypertension can encompass a wider range of underlying causes and more fully address the large number of patients who are not reaching their goals.” We suggest a need to make persistent hypertension a focus for learning health systems. @YNHH
@amjmed @YaleMed @YaleCardiology @yuan_lu1 @DrTomFrieden @YNHH "The designation of persistent hypertensions highlights need to engage these patients and address underlying causes, matching interventions to underlying causes of persistence.” Many of the causes are social, and so we need to defeat hypertension by recognizing these barriers.
@amjmed @YaleMed @YaleCardiology @yuan_lu1 @DrTomFrieden @YNHH Finally, such a learning health system approach can be supported by digital strategies to identify people falling through the cracks, & multi-disciplinary strategies to address these barriers. This is precision medicine that goes beyond life sciences to include social science.
• • •
Missing some Tweet in this thread? You can try to
force a refresh