1/
It was a delight to work with @gabifpucci of @neudrawlogy to explore the incredibly diverse CNS complications of infective endocarditis!
An #infographic & #tweetorial investigating the radiographic & clinical findings in IE + some management pearls!
#MedEd #Neurotwitter
It was a delight to work with @gabifpucci of @neudrawlogy to explore the incredibly diverse CNS complications of infective endocarditis!
An #infographic & #tweetorial investigating the radiographic & clinical findings in IE + some management pearls!
#MedEd #Neurotwitter

The most common cause of neurologic injury in IE is ischemic stroke.
But! Management is somewhat different.
Notably, due to the high risk of hemorrhagic transformation, tPA is relatively contraindicated or should be used with extreme caution.
You don’t want to end up with ⬇️!
But! Management is somewhat different.
Notably, due to the high risk of hemorrhagic transformation, tPA is relatively contraindicated or should be used with extreme caution.
You don’t want to end up with ⬇️!

3/
As evidence: in this series, 1 in 5 patients experienced post-tPA ICH and only 10% achieved a good outcome.
Thrombolysis for Ischemic Stroke Associated With Infective Endocarditis ahajournals.org/doi/full/10.11…
As evidence: in this series, 1 in 5 patients experienced post-tPA ICH and only 10% achieved a good outcome.
Thrombolysis for Ischemic Stroke Associated With Infective Endocarditis ahajournals.org/doi/full/10.11…

4/
In contrast, mechanical thrombectomy does appear to be safe in these patients. pubmed.ncbi.nlm.nih.gov/31734124/
@aneeshsinghalMD @kellysloaneMD
An example of a septic clot retrieved by mechanical thrombectomy @emoryneurocrit @emoryneurosurg image from @feras_akbik.
In contrast, mechanical thrombectomy does appear to be safe in these patients. pubmed.ncbi.nlm.nih.gov/31734124/
@aneeshsinghalMD @kellysloaneMD
An example of a septic clot retrieved by mechanical thrombectomy @emoryneurocrit @emoryneurosurg image from @feras_akbik.

5/
In addition to ischemic stroke, IE may cause cortical SAH & IPH
BOTH may be associated w/ infective intracranial aneurysms (IIAs)!
⭐️ICH in IE = vessel imaging, preferably w/ DSA ⭐️
When to screen for asymptomatic IIA?
Debatable. At least once & ideally also b/f CT Surg
In addition to ischemic stroke, IE may cause cortical SAH & IPH
BOTH may be associated w/ infective intracranial aneurysms (IIAs)!
⭐️ICH in IE = vessel imaging, preferably w/ DSA ⭐️
When to screen for asymptomatic IIA?
Debatable. At least once & ideally also b/f CT Surg

6/
The bleeding pattern resulting from ruptured IIA is often NOT the classic “aneurysmal pattern” bleed because unlike CoW aneurysms, IE aneurysms are often:
🎈Found in distal vessels
🎈Small
🎈Fusiform
pubmed.ncbi.nlm.nih.gov/29463620/ @alialawiehmdphd
Like ⬇️
The bleeding pattern resulting from ruptured IIA is often NOT the classic “aneurysmal pattern” bleed because unlike CoW aneurysms, IE aneurysms are often:
🎈Found in distal vessels
🎈Small
🎈Fusiform
pubmed.ncbi.nlm.nih.gov/29463620/ @alialawiehmdphd
Like ⬇️

7/
Infectious Endocarditis Vascular Complication Summary:
Take away 1️⃣: Treat stroke in IE with tPA at your own peril
Take away 2️⃣: Keep endocarditis on ddx when cSAH or a cortical/Sylvian fissure IPH is discovered!
Take away 3⃣: Look for the IIA.
Infectious Endocarditis Vascular Complication Summary:
Take away 1️⃣: Treat stroke in IE with tPA at your own peril
Take away 2️⃣: Keep endocarditis on ddx when cSAH or a cortical/Sylvian fissure IPH is discovered!
Take away 3⃣: Look for the IIA.
8/
Aside from vascular complications, endocarditis may also result in:
🦠intracranial abscesses
🦠meningitis
and don’t forget to also look for spinal epidural abscesses, too!
clinicalproblemsolving.com/spinal-epidura… @CPSolvers
Aside from vascular complications, endocarditis may also result in:
🦠intracranial abscesses
🦠meningitis
and don’t forget to also look for spinal epidural abscesses, too!
https://twitter.com/caseyalbin/status/1456419686195814402
clinicalproblemsolving.com/spinal-epidura… @CPSolvers
9/
Although rare, intracranial abscesses may be a delayed complication of IE… even after valve replacement & BCx clearance!
For the pt w/ persistent fevers & leukocytosis, low threshold for MRI brain to r/o abscess.
Note, these may present with just AMS!
Although rare, intracranial abscesses may be a delayed complication of IE… even after valve replacement & BCx clearance!
For the pt w/ persistent fevers & leukocytosis, low threshold for MRI brain to r/o abscess.
Note, these may present with just AMS!

10/
Check out a great @CPSolvers VMR that @gabifpucci, @shark8078Chao, @smalltownOMS, and @AaronLBerkowitz did about this topic!:
clinicalproblemsolving.com/2021/04/27/epi…
Check out a great @CPSolvers VMR that @gabifpucci, @shark8078Chao, @smalltownOMS, and @AaronLBerkowitz did about this topic!:
clinicalproblemsolving.com/2021/04/27/epi…
11/
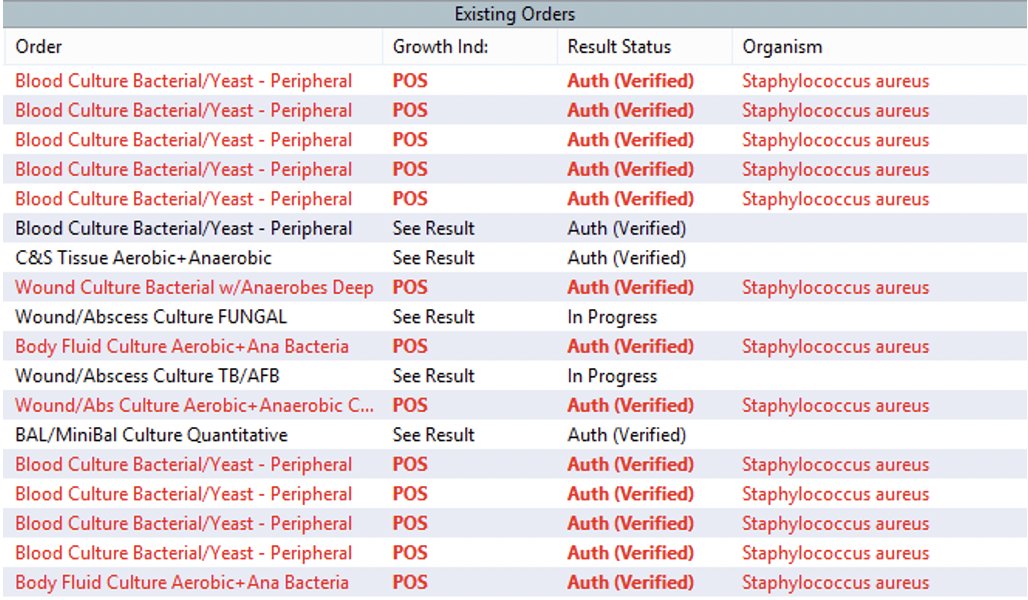
Similarly, meningitis is another infectious complication. Most commonly with S. Aureus!
The 🔑: whatever abx are being used for the endocarditis MUST have CNS penetration (no cefazolin!)
A table of abx with good CNS penetration @meganRx1 from #AcuteNeurologySurvivalGuide
Similarly, meningitis is another infectious complication. Most commonly with S. Aureus!
The 🔑: whatever abx are being used for the endocarditis MUST have CNS penetration (no cefazolin!)
A table of abx with good CNS penetration @meganRx1 from #AcuteNeurologySurvivalGuide

12/
SUMMARY:Endocarditis
🧠Can present with any number of CNS complications!
❤️Requires thoughtful approach to the timing of cardiac surgery
🧠= Low threshold for neuroimaging.
🦠Necessitates good CNS coverage!
Great reviews: tinyurl.com/sjwf7w57 tinyurl.com/km7ydhkf
SUMMARY:Endocarditis
🧠Can present with any number of CNS complications!
❤️Requires thoughtful approach to the timing of cardiac surgery
🧠= Low threshold for neuroimaging.
🦠Necessitates good CNS coverage!
Great reviews: tinyurl.com/sjwf7w57 tinyurl.com/km7ydhkf
13/
Thoughts and additions welcome! @drdangayach @rkchoi @NMatch2022 @aszelikovich @AaronLBerkowitz @WNGtweets @Tracey1milligan @harvardneuromds @EricLawson90 @sigman_md @JimmySuhMD @MariaMjaleman @MoiseyWoisey @SubinMatthews @ghoshal_shivani
Thoughts and additions welcome! @drdangayach @rkchoi @NMatch2022 @aszelikovich @AaronLBerkowitz @WNGtweets @Tracey1milligan @harvardneuromds @EricLawson90 @sigman_md @JimmySuhMD @MariaMjaleman @MoiseyWoisey @SubinMatthews @ghoshal_shivani

• • •
Missing some Tweet in this thread? You can try to
force a refresh