A #MedTwitter🧵on the frequently obtained, but ever mysterious🕵️♀️ Procalcitonin (PCT) 🦠
💡 What is it?
💡 Where does it come from?
💡 What factors/comorbid conditions may impact PCT?
#IDTwitter #TwitteRx
💡 What is it?
💡 Where does it come from?
💡 What factors/comorbid conditions may impact PCT?
#IDTwitter #TwitteRx
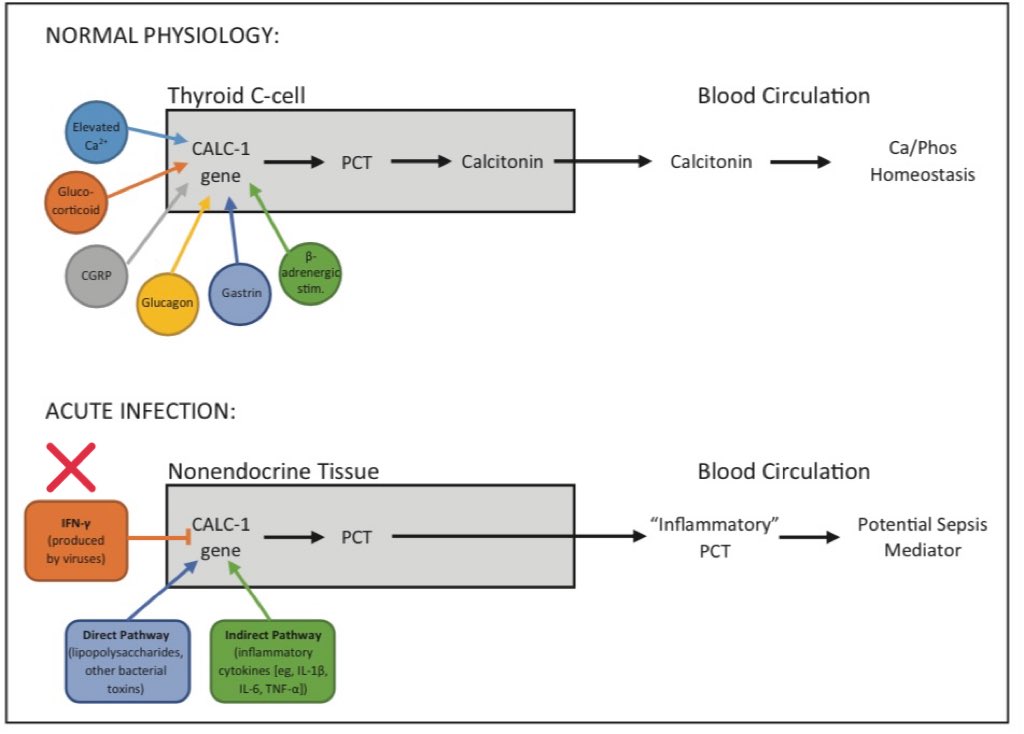
1/n First, let’s discuss the normal, physiologic role of PCT 🧬
✨116 chain amino acid
✨Neuroendocrine hormone
✨Produced by thyroid C-cells
✨Enzymatically cleaved to calcitonin
✨ Regulate Ca+2 & PO4- homeostasis
DOI 10.1093/ajhp/zxaa089
@AJHPOfficial @SESmithPharmD
✨116 chain amino acid
✨Neuroendocrine hormone
✨Produced by thyroid C-cells
✨Enzymatically cleaved to calcitonin
✨ Regulate Ca+2 & PO4- homeostasis
DOI 10.1093/ajhp/zxaa089
@AJHPOfficial @SESmithPharmD

2/n Why/How does PCT ⤴️ in bacterial infections?
✨Nonendocrine tissues (adipocytes, spleen, pancreas, etc) produce PCT but LACK 🛑 enzymes to cleave to calcitonin
✨Stimulus for non-thyroid PCT production include
1️⃣LPS/bacterial toxins ⚠️
2️⃣Cytokines (IL6, TNFa, ILb)
✨Nonendocrine tissues (adipocytes, spleen, pancreas, etc) produce PCT but LACK 🛑 enzymes to cleave to calcitonin
✨Stimulus for non-thyroid PCT production include
1️⃣LPS/bacterial toxins ⚠️
2️⃣Cytokines (IL6, TNFa, ILb)

Contrary to common belief, leukocytes only play a minor role in PCT production.
Below 👇🏻 shows a 🐁 study of tissue ⤴️ in CALC-1 gene expression in response to sepsis 🦠
doi.org/10.1210/jcem.8…
Below 👇🏻 shows a 🐁 study of tissue ⤴️ in CALC-1 gene expression in response to sepsis 🦠
doi.org/10.1210/jcem.8…

3/n Why PCT does not ⤴️ during viral 🦠 infections?
Viruses 🦠 stimulate production of INF-y
INF-y inhibits🛑CALC-1 gene expression thus PCT is not produced 💡
Viruses 🦠 stimulate production of INF-y
INF-y inhibits🛑CALC-1 gene expression thus PCT is not produced 💡
4/n What are the kinetics of PCT in bacterial infections?
From time of bacteria exposure
⏰ PCT levels ⤴️ within 3-6 hrs
⏰ PCT peaks at 6 - 14 hrs
⏰ PCT half-life = 22 - 36 hrs
Approximately 30% of PCT is cleared via the kidneys
biomerieux-diagnostics.com/sites/clinic/f…
From time of bacteria exposure
⏰ PCT levels ⤴️ within 3-6 hrs
⏰ PCT peaks at 6 - 14 hrs
⏰ PCT half-life = 22 - 36 hrs
Approximately 30% of PCT is cleared via the kidneys
biomerieux-diagnostics.com/sites/clinic/f…

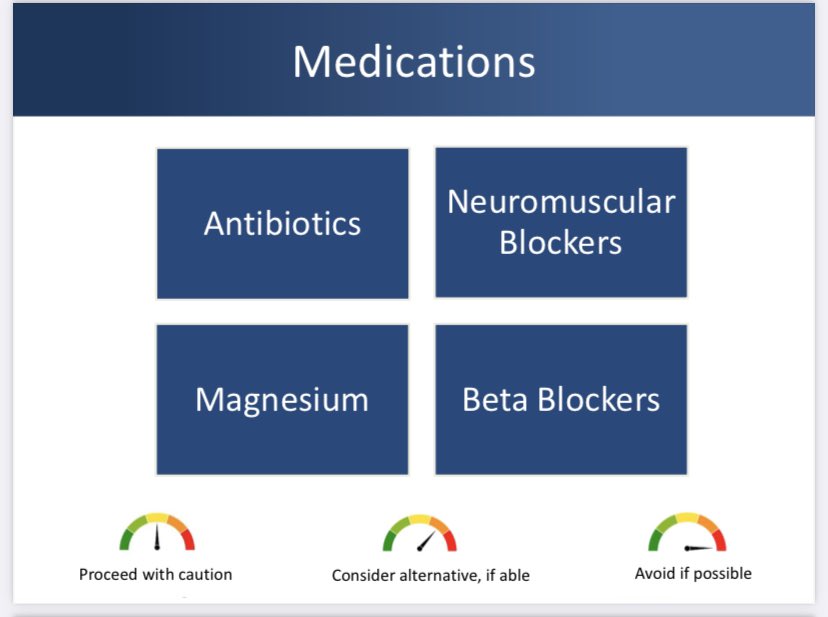
5/n What factors impact PCT levels?
⚠️ SEVERAL factors MAY impact PCT levels to varying degrees (surgery, AKI/CKD, malignancy, etc)
🔑 Assess PCT in the context of pt specific factors and other markers of infection
💡Highly recommend reading the article in tweet 1/n

⚠️ SEVERAL factors MAY impact PCT levels to varying degrees (surgery, AKI/CKD, malignancy, etc)
🔑 Assess PCT in the context of pt specific factors and other markers of infection
💡Highly recommend reading the article in tweet 1/n


6/n How to use PCT in clinical practice? 👩🏻⚕️
Remains a 🔥 topic of continued research 🔬 but as it stands currently, PCT can be a useful tool to aid in the de-escalation of ABX/ assessing response to therapy💊
📝This should NOT be used ALONE to diagnose infection
Remains a 🔥 topic of continued research 🔬 but as it stands currently, PCT can be a useful tool to aid in the de-escalation of ABX/ assessing response to therapy💊
📝This should NOT be used ALONE to diagnose infection
Concluding thoughts 💭on PCT
✨PCT produced via nonendocrine tissues in response to bacterial infection
✨Useful to differentiate btwn bacterial vs viral inf 🦠
✨Impacted by various factors/conditions, thus not be used alone to 👀 for inf
🧵 inspired by @pouyeah
✨PCT produced via nonendocrine tissues in response to bacterial infection
✨Useful to differentiate btwn bacterial vs viral inf 🦠
✨Impacted by various factors/conditions, thus not be used alone to 👀 for inf
🧵 inspired by @pouyeah
• • •
Missing some Tweet in this thread? You can try to
force a refresh