Alert 🎙Pharmacy Grand Rounds Thread Ahead! 🚨
Last week I had one of my final presentations of the year! With a catchy title😉
Urine for an Update! Updates in the management of metastatic urothelial cancer
Hold your bladders, this is an extensive update! 😂
#oncopharm
Last week I had one of my final presentations of the year! With a catchy title😉
Urine for an Update! Updates in the management of metastatic urothelial cancer
Hold your bladders, this is an extensive update! 😂
#oncopharm

Bladder cancer can be divided into two ✌️subtypes:
1) Non-muscle invasive: encompasses in-situ and localized disease➡️5-yr OS >70%
2) Muscle invasive: encompasses regional or metastatic disease➡️5-yr OS dismal especially for metastatic disease 😔
1) Non-muscle invasive: encompasses in-situ and localized disease➡️5-yr OS >70%
2) Muscle invasive: encompasses regional or metastatic disease➡️5-yr OS dismal especially for metastatic disease 😔

Cisplatin=SOC
50% of pts w are ineligible due to older age👵🏻, poor PS, ⬇️ renal function, ⬇️hearing, neuropathy, heart failure 🫀& other comorbities that ⬆️ risk of ⚠️
Carboplatin yields inferior responses➡️NOT 🙅🏻♀️ an equal alternative due to ⬇️ OS😢➡️pt left w/minimal tx options
50% of pts w are ineligible due to older age👵🏻, poor PS, ⬇️ renal function, ⬇️hearing, neuropathy, heart failure 🫀& other comorbities that ⬆️ risk of ⚠️
Carboplatin yields inferior responses➡️NOT 🙅🏻♀️ an equal alternative due to ⬇️ OS😢➡️pt left w/minimal tx options

Luckily 👍🏼 there has been a tsunami 🌊 of new therapies approved for mUC in the recent decade: my presentation discussed the orange treatments in detail below! 
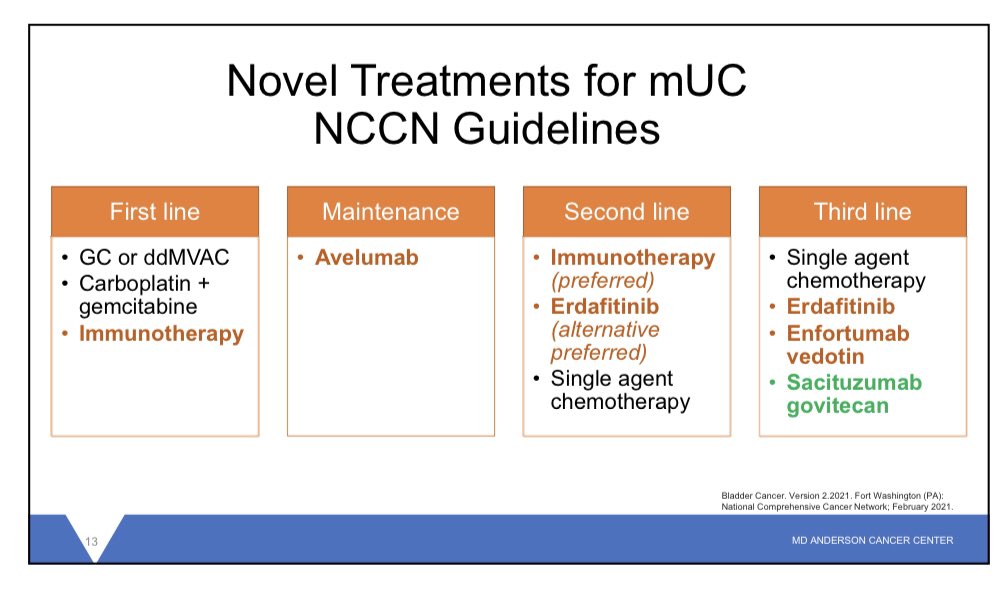
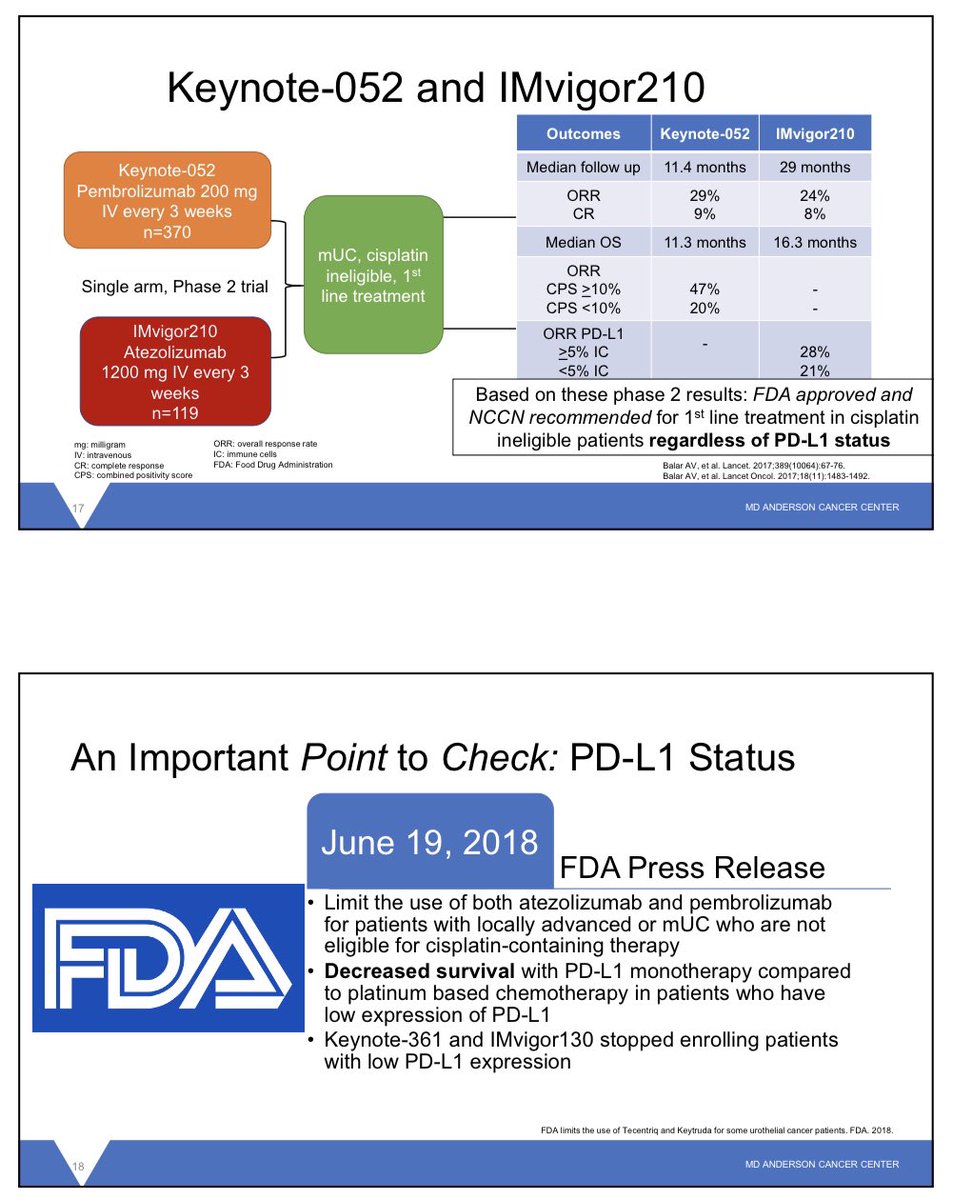
1st: Pembro/Atezo to provide pts who are cisplatin inelidgble improved tx💊options
✅median OS > what we see 👀 with carbo (‼️indirect comparison‼️)
However an important POINT to CHECK(no pun intended)is PDL1 status➡️indicated only for PDL1+ pts unless ineligible for all chemo
✅median OS > what we see 👀 with carbo (‼️indirect comparison‼️)
However an important POINT to CHECK(no pun intended)is PDL1 status➡️indicated only for PDL1+ pts unless ineligible for all chemo
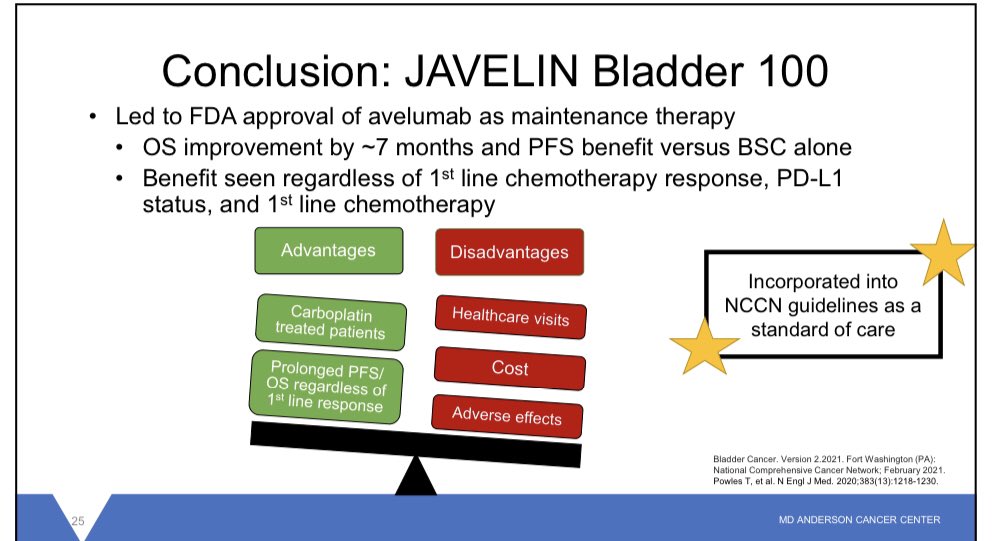
The most predominant advancement in mUC is maintenance avelumab
JAVELIN Bladder 100➡️7 month improvement 🏆in OS compared to BSC➡️1st maintenance therapy for mUC!
Please 👀 advantages and disadvantages below!
JAVELIN Bladder 100➡️7 month improvement 🏆in OS compared to BSC➡️1st maintenance therapy for mUC!
Please 👀 advantages and disadvantages below!
💊1st targeted🎯tx for mUC‼️
Erdafitinib➡️pan-FGFR inhibitor❌approved for 2nd/3rd line mUC in for pts w/ susceptible FGFR3/2 genetic alterations
FGFR expressed in ~15% of mUC pts, studied in phase 2 trial BLC2001 ORR of 40% (improved ORR vs chemotherapy which yields~8-13% ORR)
Erdafitinib➡️pan-FGFR inhibitor❌approved for 2nd/3rd line mUC in for pts w/ susceptible FGFR3/2 genetic alterations
FGFR expressed in ~15% of mUC pts, studied in phase 2 trial BLC2001 ORR of 40% (improved ORR vs chemotherapy which yields~8-13% ORR)

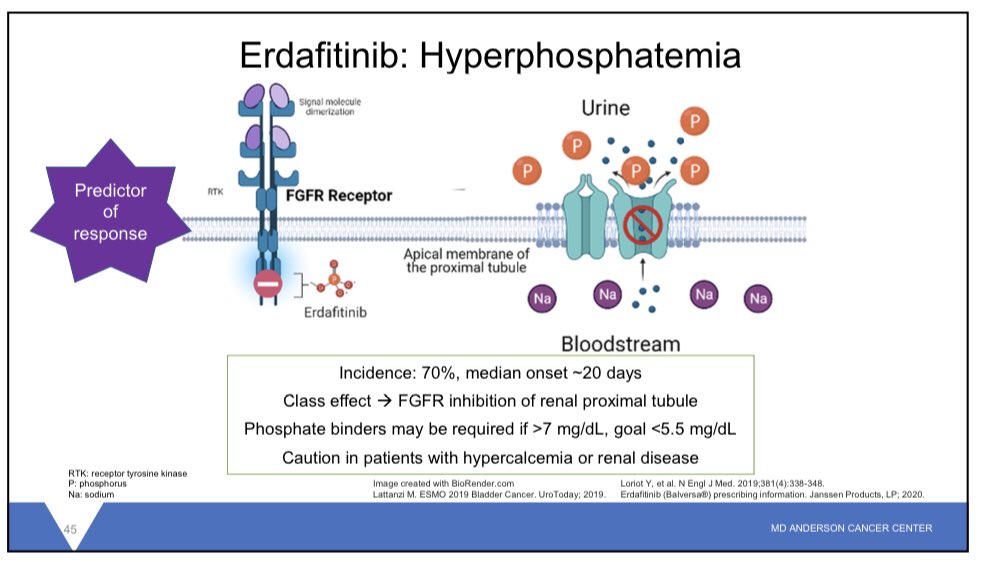
One☝🏻cool😎 fact about erdafitnib➡️FGFR found in apical membrane of renal tubules➡️❌exchange of Phos/Na leading to hyperphosphatemia (👀👇🏻)
Interestingly🧐associated w/tx response😮
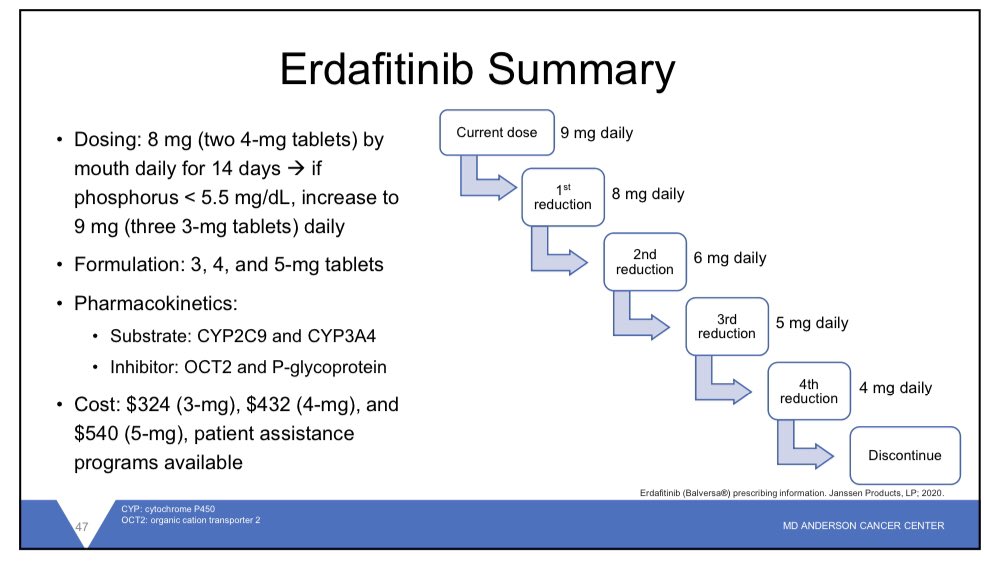
Dose titration req (8mg/d➡️14 days➡️9mg/d if phos <5.5mg/dL)
⚠️caution renal imp or hyperCa⚠️

Interestingly🧐associated w/tx response😮
Dose titration req (8mg/d➡️14 days➡️9mg/d if phos <5.5mg/dL)
⚠️caution renal imp or hyperCa⚠️
Enfortumab-vedotin: antibody-drug conjugate🎯nectin-4 (expressed in 93% of mUC) bound to MMAE (microtubule distrusting agent🧬)
EV-301 phase 3 trial of EV in the 3L setting➡️30% RR for death 🤯
Ongoing studied looking at EV in earlier lines of tx & combined with immunotherapy!

EV-301 phase 3 trial of EV in the 3L setting➡️30% RR for death 🤯
Ongoing studied looking at EV in earlier lines of tx & combined with immunotherapy!
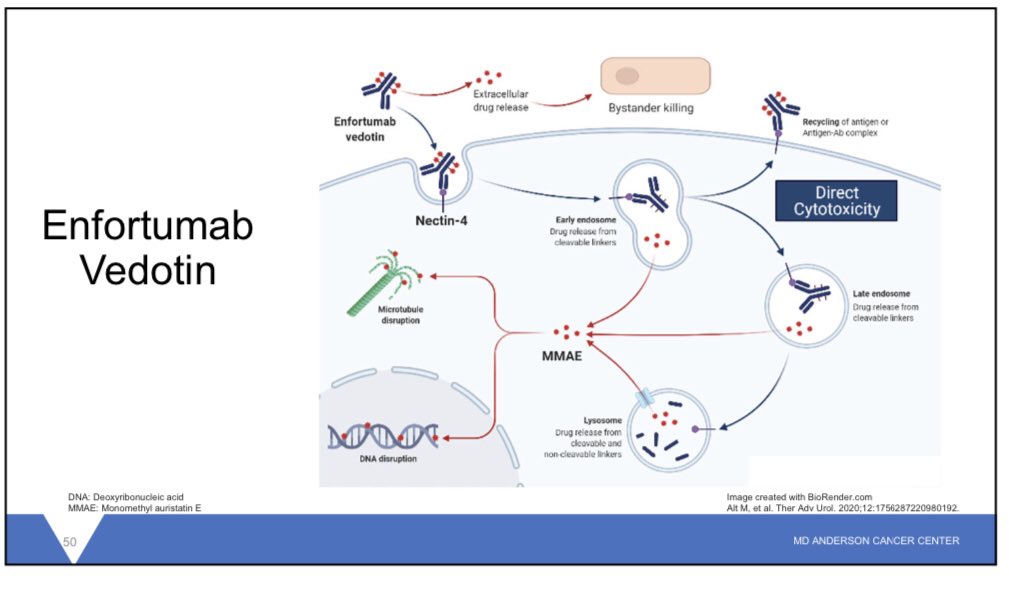

Big AE to monitor for with EV are
1️⃣Hyperglycemia🍭(1💀 due to DKA on trial)
2️⃣ 👀disorders (dry eye, keratitis: Rx💊ocular steroid)
3️⃣Neuropathy: like brentuximab-VEDOTIN, the MMAE results in peripheral neurop
4️⃣Skin: nectin-4 expressed ubiquitously in skin➡️🔎 for SJS/TEN⚠️
1️⃣Hyperglycemia🍭(1💀 due to DKA on trial)
2️⃣ 👀disorders (dry eye, keratitis: Rx💊ocular steroid)
3️⃣Neuropathy: like brentuximab-VEDOTIN, the MMAE results in peripheral neurop
4️⃣Skin: nectin-4 expressed ubiquitously in skin➡️🔎 for SJS/TEN⚠️
How to decide between novel therapies? 🧐
✅Favors EV: retinal disorder (BBW for central serous retinopathy for erda), concern for adherence, absent FGFR (only found in 15%!), CKD/hyperCa due to hyperphosphatemia risk
✅Favors erdafitnib: uncontrolled DM, prefers oral tx, PN!
✅Favors EV: retinal disorder (BBW for central serous retinopathy for erda), concern for adherence, absent FGFR (only found in 15%!), CKD/hyperCa due to hyperphosphatemia risk
✅Favors erdafitnib: uncontrolled DM, prefers oral tx, PN!

Thank you for viewing! Feel free to add your thoughts💭 about novel updates in mUC! #oncopharm #bladdercancer #immunoOncology #TwitteRx
• • •
Missing some Tweet in this thread? You can try to
force a refresh