ICU stories: Middle-aged pt w PMHx of rheum fever/A fib underwent MV+AV replacement, TV repair w ring, Maze procedure + LA appendage closure. At the end of surgery, TEE was “fine”; pt was transferred to the ICU intubated (fio2 40%) on low-dose levo (0.04). Could not be extubated
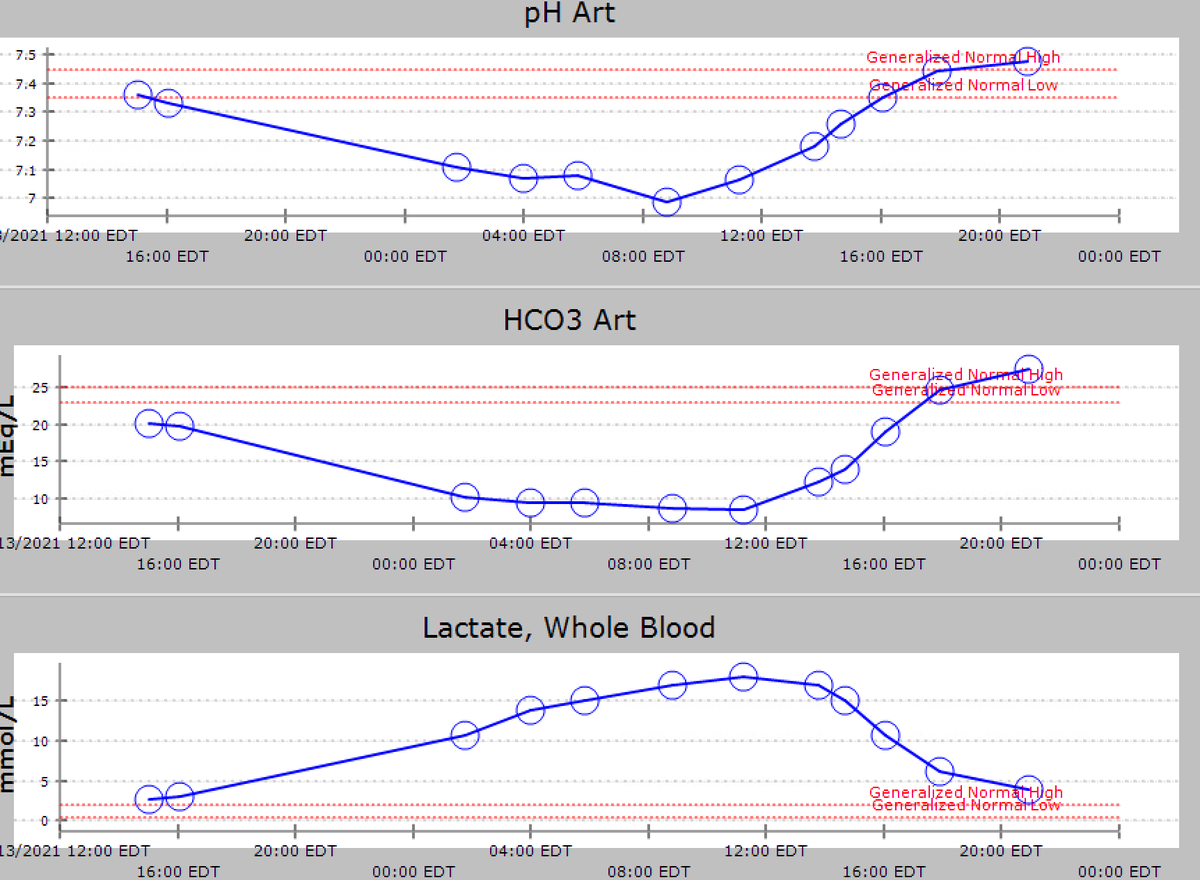
because few h later, lactate began to ⬆️ and ivf were given. Levo gtt did not ⬆️ much (just @ 0.1 next am) but lactate was up to 17 mmol/l & pH was 6.98. I was told that pt was probably still "under-resuscitated". When I 👀the chart, pt had received multiple NS, bicarb & albumin
boluses and was > 8 liters positive. I first pulled the bed sheets to look at the legs and feel the skin temp: 

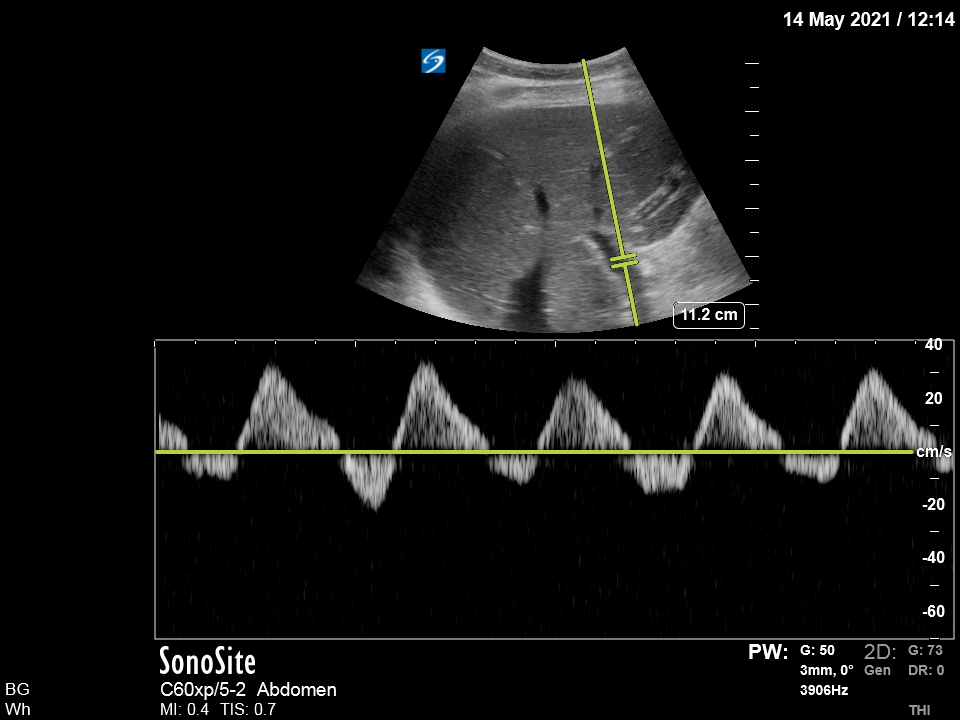
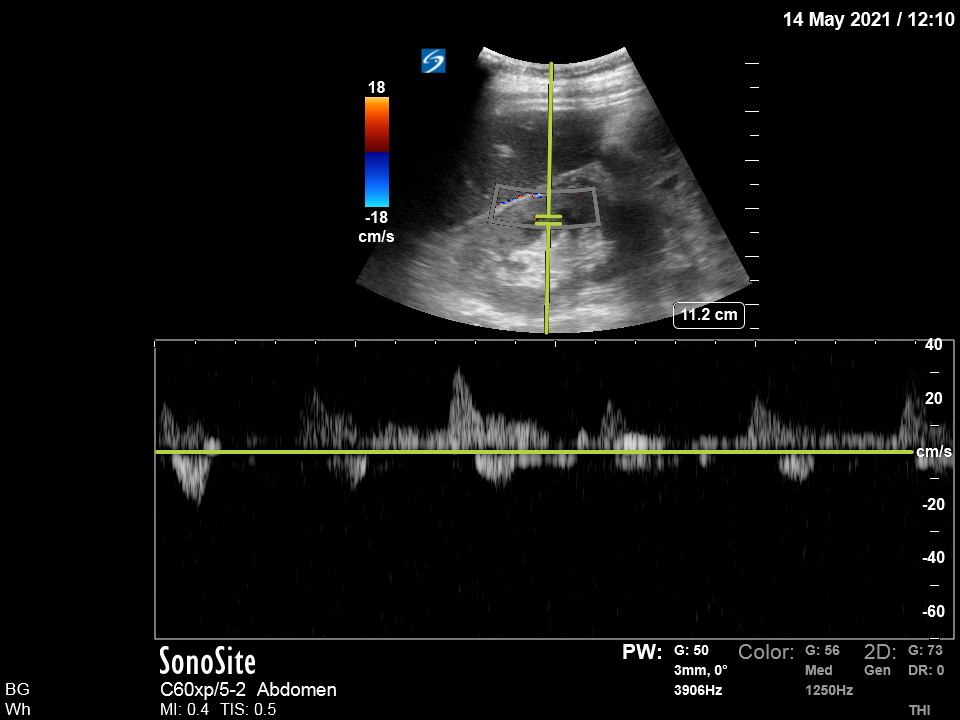
POCUS was the next step. Obviously very poor images, but can still make an assessment:
LV had low normal systolic function, RV function was reduced, valves looked "ok", and there was no pericardial effusion. TAPSE was 8 mm (normal > 17). I then did a "color" VEXUS (first 3 sec: PV; then: HVs):
I found: prominent hepatic veins w diastolic flow / portal vein w > 100% pulsatility. Renal vein Doppler revealed monophasic pattern. Pt was obviously in cardiogenic shock due to RV failure and went to cath lab where a RHC showed: 
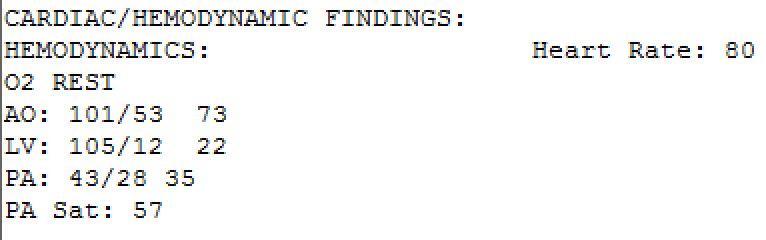
An Impella RP was inserted; this is a RV assist device that can provide temporary RV support for up to 2 wks in pts who develop acute R heart failure following open-heart surgery etc. This clip from that day:
The RP inflow is positioned in the IVC and the outflow in the L pulmonary artery; thus, it aspirates blood from the IVC and expels it into the PA at a flow up to 4 L/min. Swan-Ganz is placed in the R PA (this is from the same pt): 

The same night CRRT was started as pt had become anuric. When I repeated VEXUS that night, the HV/PV pulsatilities were gone. The following portal vein color Doppler clip is from next am:
Flat hepatofugal HV (below baseline) and hepatocentral PV (above baseline; the dip is probably due to inspiratory effort and vessel translation away off my probe): 



My first -naive?- impression was that RV was much better and this eliminated all pulsatility. Now, I think that since Impella RP is a big 22 French catheter/pump occupying big part of the TV annulus and the IVC diameter, it may just not allow the upstream transmission of pulses!
Unfortunately, and despite the initial improvement of hemodynamics post Impella placement, pt was already in MOF (renal - liver - coagulopathy) and died days later
Take-home messages:
1. The lacto-bolo reflex (the reflexive administration of iv fluids in response to a rising lactate) can be very dangerous.
2. A post open-heart surgery pt is much more likely to have a cardiogenic cause of "crashing" than just volume depletion.
1. The lacto-bolo reflex (the reflexive administration of iv fluids in response to a rising lactate) can be very dangerous.
2. A post open-heart surgery pt is much more likely to have a cardiogenic cause of "crashing" than just volume depletion.
3. VEXUS can fill the missing pieces of hemodynamic puzzles in ambulatory as well as crashing and burning postop patients.
As always, thanks for reading!
As always, thanks for reading!
Special thanks to those who keep pushing the envelope of #VEXUS #POCUS #ECHOFIRST #FOAMed #FOAMus #FOAMcc #IMPOCUS #MedEd : @NephroP @ArgaizR @ThinkingCC @Thind888 @katiewiskar @khaycock2 @EM_RESUS @msenussiMD @msiuba @PulmCrit @MDBeni @iceman_ex
@thepocusatlas @HeyDrNik @ICUltrasonica @NickjohnsonMD @EmergenxyPhysic @DraHuerta09 @pocusmeded @POCUSClub @thepocusatlas @AmbrizMau @ecocritic_es @TaotePOCUS @Pocus101 @VelezNephHepato @pocusfoamed @interconsulta @EmergencyEcho @echotalk @cianmcdermott @ImagenCardiaca
@apenarEM @PorrosE @chileanestesia @vaszochios @nickmmark @cjosephy @The_echo_lady @pdsalinas @GUH_ICU_Anaesth @KalagaraHari @UAlberta_Sono @EMUGs_ @UAlberta_ICU @UAB_Sono @MonaresTI @EMUGs_ @MedCriticaMex @critconcepts @pablitorf @MediCasos @ultra2ente @ACEP_EUS
@grepmeded @ImagenCardiaca @RosenelliEM @FisioPocus #EMBound @ACEP_EUS @MetroHealth_EM @MH_EMultrasound @jminardi21 @RJonesSonoEM @jaffa_md @kyliebaker888 @TomJelic @siddharth_dugar
The first 3 sec were from HV color doppler and the last 3 sec from PV. But you know this already.
• • •
Missing some Tweet in this thread? You can try to
force a refresh