1/ I'm really excited that the @US_FDA has granted an EUA for #Paxlovid - this is a terrific new option for #OmicronVariant and kudos to the scientists, researchers, and developers at Pfizer. So timely, and so necessary as we face a wave of new #COVID19 infections globally.
2/ I went through the fact sheet and it is critical to highlight that many patients with cancer and organ transplant recipients are on medications that will be effected by the #ritonavir component of #paxlovid.
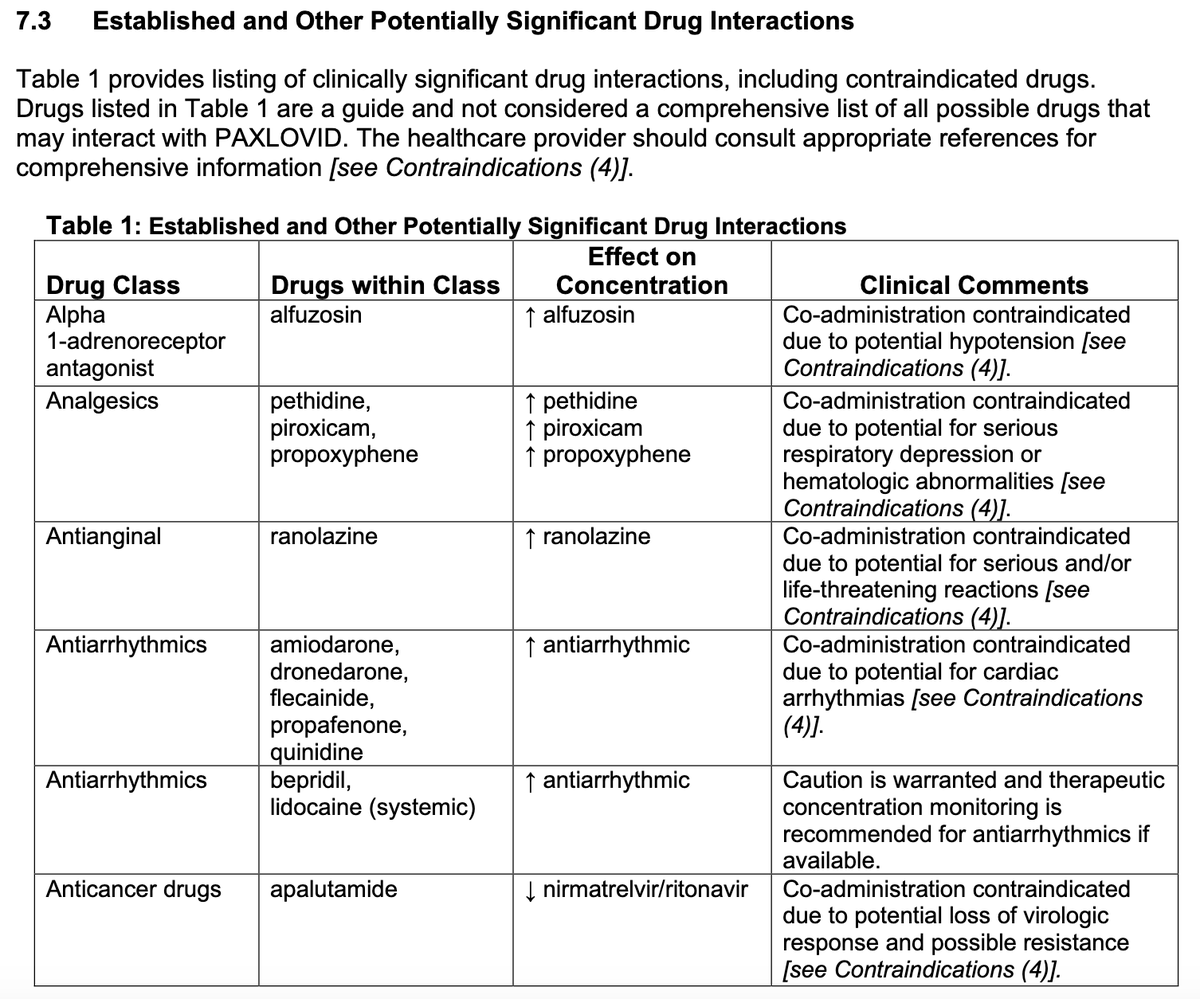
3/ Note black box warning - Co-administration of ritonavir with sedative hypnotics, anti-arrthythmics, or ergot alkaloids are contraindicated.
Pfizer did a great job in compiling potential drug-drug interactions:
Pfizer did a great job in compiling potential drug-drug interactions:
10/ Unlike ritonavir in HIV medicine, #paxlovid will be a short course (5 days). This may mitigate some of the drug-drug interactions. However, #IDTwitter and #TxID needs to help educate non-ID physicians on the use and potential interactions of protease inhibitor therapy.
11/ Full fact sheet here: fda.gov/media/155050/d…
As ID practitioner with lots of patients on calcineurin inhibitors, ibrutinib and other -nibs, azoles etc, I am curious how other ID docs will take this into account when faced with a newly diagnosed #COVID19 patients.
As ID practitioner with lots of patients on calcineurin inhibitors, ibrutinib and other -nibs, azoles etc, I am curious how other ID docs will take this into account when faced with a newly diagnosed #COVID19 patients.
12/ As a general rule, I treat a proven infection with the most effective drug and deal with side effects and DDIs as they arise. I never want to withhold the most effective therapy for theoretical concerns. @EricTopol @FungalDoc @GermHunterMD @IdVilchez @mini_kamboj @LionakisLab
13/ @PergamIC @JoshuaHillMD @BradSpellberg @roby_bhatt @sloan_kettering @DrMiguelPerales @EBabady @evrnyc @rosslevinemd @gilles_salles @LesokhinMD @szusmani @ZainabShd
15/ For the primary outcome listed here (COVID-19 related hospitalization or death through day +28), the number needed to treat to prevent one event is approximately 18.
• • •
Missing some Tweet in this thread? You can try to
force a refresh











