1/ We are all seeing the massive wave of Omicron sweep through our communities
Severity will make the difference between a bad winter and a horrific one
We keep saying "hospitalizations are still low, but it's early"
When is it time?
In NYC, it should be showing now.
Severity will make the difference between a bad winter and a horrific one
We keep saying "hospitalizations are still low, but it's early"
When is it time?
In NYC, it should be showing now.

2/ If you look at the counts of COVID cases and subsequent hospitalizations, they tend to track each other quite closely, but with a lag of 5-6 days
Deaths follow hospitalizations, by about 12 days. (it's too soon for that)
[Big props to my alma mater @nycHealthy for #opendata]
Deaths follow hospitalizations, by about 12 days. (it's too soon for that)
[Big props to my alma mater @nycHealthy for #opendata]
3/ So how many hospital admissions should we be seeing right now?
First, let's look at what's happened to the hospitalization rate in NYC since the awful days of March 2020.
It's gotten a LOT better (in part because we're better at testing and diagnosing COVID)
First, let's look at what's happened to the hospitalization rate in NYC since the awful days of March 2020.
It's gotten a LOT better (in part because we're better at testing and diagnosing COVID)

4/ In March/April 2020, looking at lagged hospital admissions vs cases reported, the ratio is 21%
You had to be pretty sick or lucky to get a COVID test
By the Alpha wave, it was down to 6.9% (less testing explains the super quiet summer bump)
Vaccines have two effects ...
You had to be pretty sick or lucky to get a COVID test
By the Alpha wave, it was down to 6.9% (less testing explains the super quiet summer bump)
Vaccines have two effects ...
5/ During this fall's Delta surge, vaccines protected a large part of the City's population from infection (reducing cases), but with an even bigger impact on severe illness, esp among the elderly
So the net is that hospitalization rate dropped to 4.9%
That's our baseline
So the net is that hospitalization rate dropped to 4.9%
That's our baseline

6/ The Omicron surge in hospitalizations in NYC started its climb on December 13th.
(Only 11 days ago, but these have been long days)
From December 13-16th there were 42,624 cases by report date
(NYC provides different dataset with diagnosis date as well- 38,113 in that span)
(Only 11 days ago, but these have been long days)
From December 13-16th there were 42,624 cases by report date
(NYC provides different dataset with diagnosis date as well- 38,113 in that span)

7/ So we would a 5% hospitalization rate after a 5 day lag if Omicron follows the same impact as Delta on the NYC population.
That pencils out to between 1,870 and 2,090 expected hospital admissions.
we had 780.
That's about 58-63% less than expected
Confounders? a few
That pencils out to between 1,870 and 2,090 expected hospital admissions.
we had 780.
That's about 58-63% less than expected
Confounders? a few
8/ We are probably undercounting cases
It's hard to get a PCR test in NYC right now, and so many more infections are going undiagnosed, or diagnosed only with rapid antigen kits, that aren't reported to public health
That would means an even lower hospitalization rate/ severity
It's hard to get a PCR test in NYC right now, and so many more infections are going undiagnosed, or diagnosed only with rapid antigen kits, that aren't reported to public health
That would means an even lower hospitalization rate/ severity

9/ We may be over-counting COVID hospitalizations
A high attack rate for Omicron means a higher likelihood that patients will be incidentally found to be infected WITH omicron, not FROM it
Maybe 20% of COVID admits? That would mean a lower severity rate
samrc.ac.za/news/tshwane-d…
A high attack rate for Omicron means a higher likelihood that patients will be incidentally found to be infected WITH omicron, not FROM it
Maybe 20% of COVID admits? That would mean a lower severity rate
samrc.ac.za/news/tshwane-d…
10/ Finally, some of the COVID infections may actually still be Delta rather than Omicron, which would also imply a lower hospitalization rate for omicron itself
So based on early returns, it does seem that 3% or fewer of Omicron cases will be hospitalized
That could be a lot
So based on early returns, it does seem that 3% or fewer of Omicron cases will be hospitalized
That could be a lot
11/ The hospital mortality rate for COVID was 29% during the awful March-April 2020 period, and has come down to 18% since with better protocols and less overwhelmed staff
But if hospital capacity falls as cases rise, it could get bad
CDC action today helpful given omicron
But if hospital capacity falls as cases rise, it could get bad
CDC action today helpful given omicron

12/ Back of envelope- If Omicron surge and fall takes place over the next 6 weeks, could see something like 1.2M NYers infected, maybe 400,000 diagnosed
Even a 3% hospitalization rate would mean 12,000 hospitalizations (more than all NYS empty bed capacity rn), over 2,000 deaths
Even a 3% hospitalization rate would mean 12,000 hospitalizations (more than all NYS empty bed capacity rn), over 2,000 deaths
13/ That's a far cry from Mar-Apr 2020 when over 25,000 perished, but is what you might expect from a bad influenza season (which we might have as well this year)
As always, we need to get boosters in arms (esp nursing homes), N95 masks for high risk, and try to ride it out 🙏
As always, we need to get boosters in arms (esp nursing homes), N95 masks for high risk, and try to ride it out 🙏
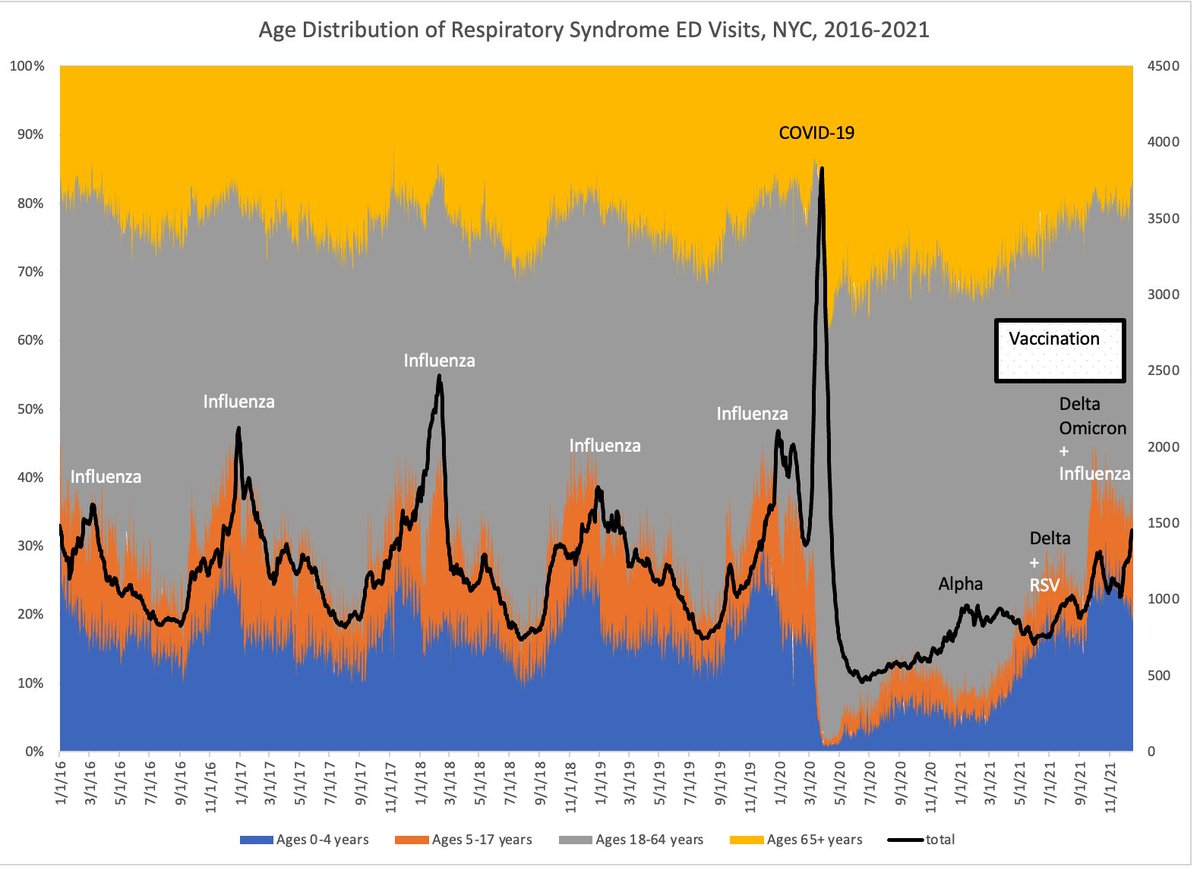
14/ [NB: I would have liked to add a comparison to Emergency Department Respiratory Syndrome visits, but the website is down??
After years of working reliably with mostly benign neglect this moment seems like terrible timing to be messing with it]
After years of working reliably with mostly benign neglect this moment seems like terrible timing to be messing with it]

15/ Many thanks to friends on this website for adding great comments and links to other data analyses. I will add them to the thread for broader visibility
*Excellent analysis of "incidentals" from the UK (rising, ~30% of total) from @jburnmurdoch
*Excellent analysis of "incidentals" from the UK (rising, ~30% of total) from @jburnmurdoch
https://twitter.com/jburnmurdoch/status/1473982353580175365?t=oTGXwIguP-R32yvwxEFmiA&s=19
16/ great point by @reichlab - preholiday testing may be catching infections sooner, could push out the usual relationship between cases and hospitalizations.
(Also read his thread using similar cross correlation analysis to find 3-5 day lag nationally)
(Also read his thread using similar cross correlation analysis to find 3-5 day lag nationally)
https://twitter.com/reichlab/status/1473286827889020932?t=Xoxrs3YBSPW7CBgsGl_huw&s=19
17/ a caution
I'm talking specifically about NYC, a highly vaccinated community
Per @Bob_Wachter, SF has perhaps an even greater dissociation between cases and admissions.
But if the relatively lower severity is due to vaccines, then less vacc communities would be hit harder
I'm talking specifically about NYC, a highly vaccinated community
Per @Bob_Wachter, SF has perhaps an even greater dissociation between cases and admissions.
But if the relatively lower severity is due to vaccines, then less vacc communities would be hit harder
• • •
Missing some Tweet in this thread? You can try to
force a refresh