It's 5:45 in the morning and I'm coming up to the final few hours of my afternoon/evening/overnight shift. Things have changed since last week, and here's where we're at.
/1
#Omicron #COVID19 @HRHospital
/1
#Omicron #COVID19 @HRHospital

The first observation is that the ER team at my hospital are absolute heroes, and I don't say that lightly. They are taking the brunt of the Omicron wave both in terms of patient volume and exposure to the virus. They do all of this with calm professionalism.
/2
/2

This takes me directly to the real crisis that's been brewing this wave. Due to the highly contagious nature of Omicron, we're slowly losing frontline staff. The stress for those remaining is not from fear of catching the virus, but fear of being stretched too thin.
/3
/3

So what is coming through the ER? COVID. Lots and lots of COVID, and it's all Omicron.
Like last week, most of the patients are symptomatic, but not seriously ill. They have typical flu like symptoms.
Some however are extremely sick.
/4
Like last week, most of the patients are symptomatic, but not seriously ill. They have typical flu like symptoms.
Some however are extremely sick.
/4

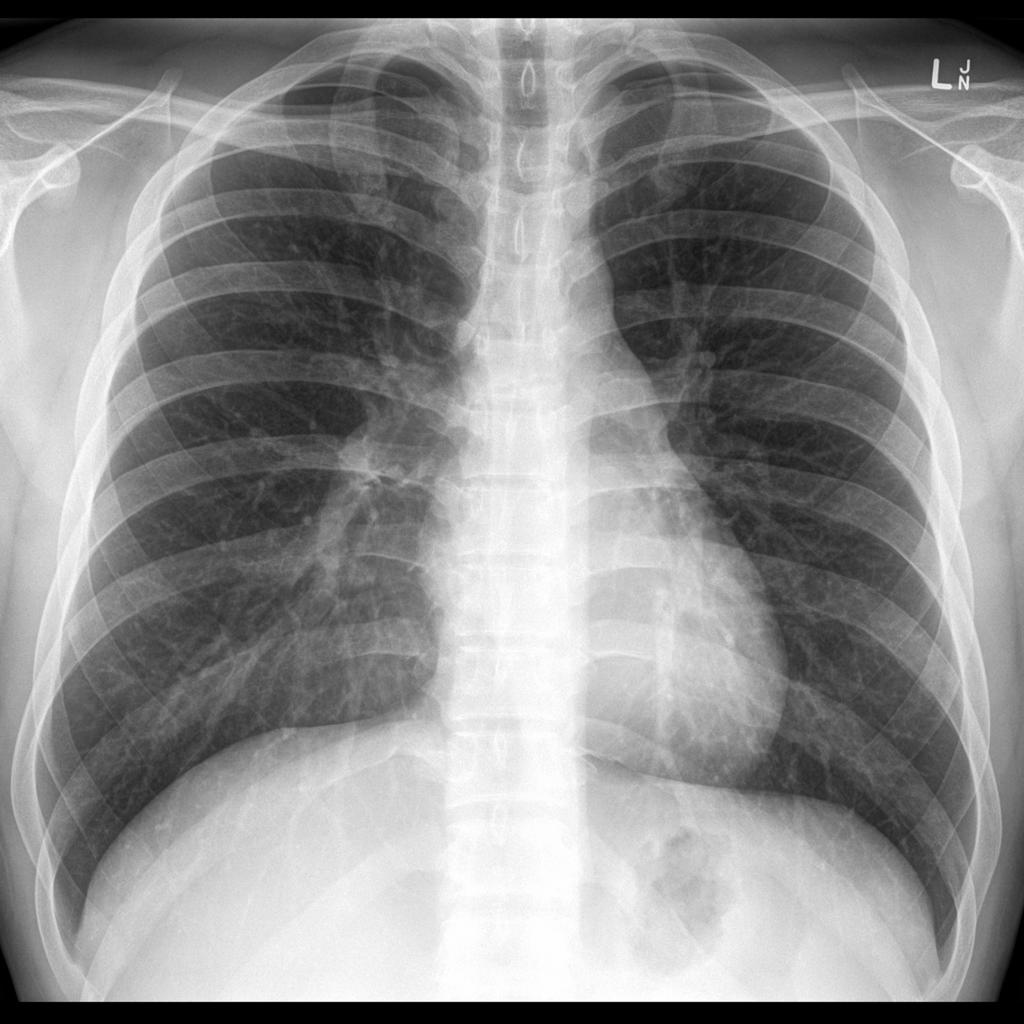
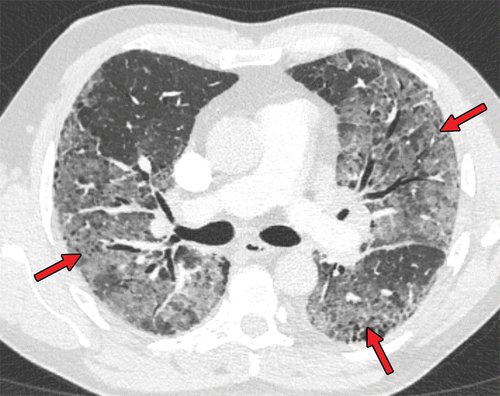
What do Omicron patients look like on imaging?
The vast majority of the chest X-rays coming through on these patients are normal. A small number show very mild pneumonias which are less severe than in previous waved.
A very small number are downright horrible.
/5
The vast majority of the chest X-rays coming through on these patients are normal. A small number show very mild pneumonias which are less severe than in previous waved.
A very small number are downright horrible.
/5

The normal X-rays and the near normal ones belong to younger patients and vaccinated patients of all ages. There are vanishingly few pediatric cases with pneumonias.
The horrible pneumonias are seen in the unvaccinated, the immunosuppressed, and some elderly patients.
/6
The horrible pneumonias are seen in the unvaccinated, the immunosuppressed, and some elderly patients.
/6

What's changed in a week is volume. The number of patients coming through ER remains ridiculous, but few need imaging and fewer need admission.
The number of mild pneumonias has roughly doubled. The number of severe pneumonias is also up slightly.
/7
The number of mild pneumonias has roughly doubled. The number of severe pneumonias is also up slightly.
/7
Based on volume alone, this has increased our inpatient numbers with COVID, but it's not as simple as that.
The numbers can be broken down further to give us some interesting insights into Omicron.
/8
The numbers can be broken down further to give us some interesting insights into Omicron.
/8
Our 744 bed hospital now has 80 COVID positive patients, 9 of which are in the ICU.
60% of the ward patients are in because of COVID, while 40% are in hospital for other reasons.
78% of ICU patients are admitted for COVID. 22% in ICU are admitted for other reasons.
/9
60% of the ward patients are in because of COVID, while 40% are in hospital for other reasons.
78% of ICU patients are admitted for COVID. 22% in ICU are admitted for other reasons.
/9
The age distribution is also telling. Omicron is unkind to our older population.
29% of inpatients with COVID are 60-79yrs old.
41% of inpatients with COVID are 80yrs old, or older.
/10
29% of inpatients with COVID are 60-79yrs old.
41% of inpatients with COVID are 80yrs old, or older.
/10

How can you use this information?
1. Get vaccinated and boosted. Omicron is a disease of the unvaccinated.
2. If you are unvaccinated, elderly, or immunosuppressed, be cautious. Wear a high quality mask, and avoid crowds.
3. EVERYONE is catching Omicron, so don't be cocky
/10
1. Get vaccinated and boosted. Omicron is a disease of the unvaccinated.
2. If you are unvaccinated, elderly, or immunosuppressed, be cautious. Wear a high quality mask, and avoid crowds.
3. EVERYONE is catching Omicron, so don't be cocky
/10

What does this mean for the next few weeks?
The walking wounded make up the majority of Omicron patients. Few end up in hospital. Hospitals are unlikely to be overwhelmed by patients.
The staffing shortages are however going to cause capacity problems in the short term.
/11
The walking wounded make up the majority of Omicron patients. Few end up in hospital. Hospitals are unlikely to be overwhelmed by patients.
The staffing shortages are however going to cause capacity problems in the short term.
/11

Final point? It will be impossible to predict what will peak first, staffing shortages, or the Omicron wave. So if you have mild flu like symptoms, assume you have Omicron, and STAY OUT OF THE EMERGENCY ROOM.
Let's minimize their exposure and keep ahead of the wave.
/12
Let's minimize their exposure and keep ahead of the wave.
/12

• • •
Missing some Tweet in this thread? You can try to
force a refresh