The more you understand, the less you need to memorize. Take this 🫀 example:
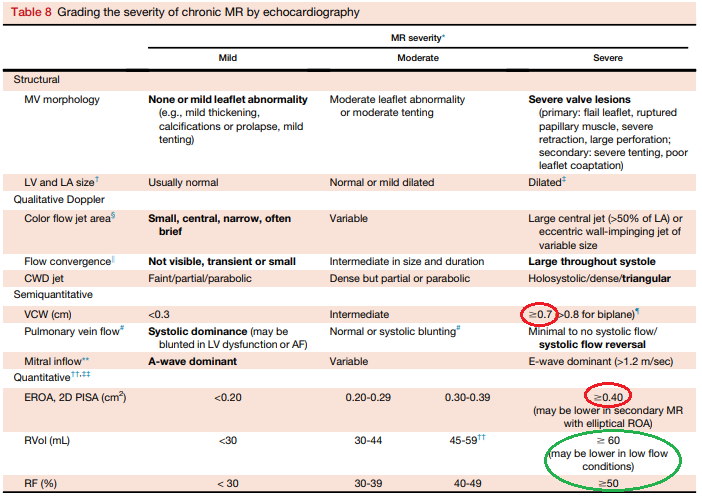
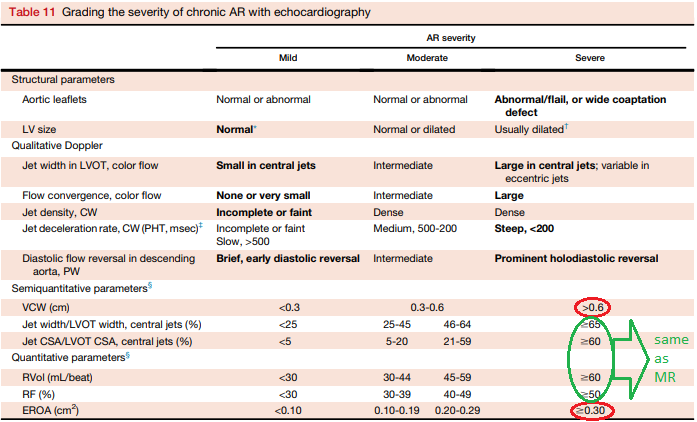
Severe AR and MR are both defined by a regurgitant volume of 60mL. YET, another criterion, effective orifice area, must be 0.3cm^2 for AR but 0.4 for MR.
#Medtwitter #cardiotwitter #POCUS #Echofirst
Severe AR and MR are both defined by a regurgitant volume of 60mL. YET, another criterion, effective orifice area, must be 0.3cm^2 for AR but 0.4 for MR.
#Medtwitter #cardiotwitter #POCUS #Echofirst
I kept mixing up which is 0.3 and which is 0.4. We can keep trying to memorize this, or ask why? Why is the regurgitant volume the same, but the effective regurgitant orifice area (EROA) different?
Here's the pearl:
Here's the pearl:
It's because AR occurs in diastole, MR occurs in systole, and diastole is longer than systole. Therefore, in diastole, a smaller EROA (0.3) can generally yield the same 60mL of regurgitation as a larger EROA (0.4) can during the shorter systole.
Sure, there's still numbers to memorize, and digging further can help memorize even less. But for now, for those like myself mixing up which is 0.3 and which is 0.4, it should hopefully no longer be an issue.
#CCEeXAM @CardioNerds @msiuba @NephroP @nickmmark
#CCEeXAM @CardioNerds @msiuba @NephroP @nickmmark
Addendum:
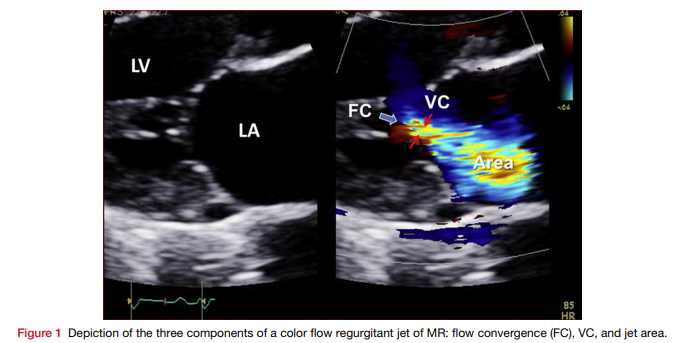
AR is also defined by a vena contracta (VC) of 6mm, yet MR requires 7. This is likely for the same reason:
Diastole requires a smaller EROA *and* VC to achieve the same regurg. volume as a larger EROA & VC in the shorter systole.
More simply, larger EROA = larger VC.


AR is also defined by a vena contracta (VC) of 6mm, yet MR requires 7. This is likely for the same reason:
Diastole requires a smaller EROA *and* VC to achieve the same regurg. volume as a larger EROA & VC in the shorter systole.
More simply, larger EROA = larger VC.
• • •
Missing some Tweet in this thread? You can try to
force a refresh