Today I virtually lectured the residents from @BCM_PMandR & @UTHPMR about #LongCOVID.
I was touched that the residents wanted the slides & thought it was one of the most important talks of the year. Will share some in a thread 🧵
I was touched that the residents wanted the slides & thought it was one of the most important talks of the year. Will share some in a thread 🧵

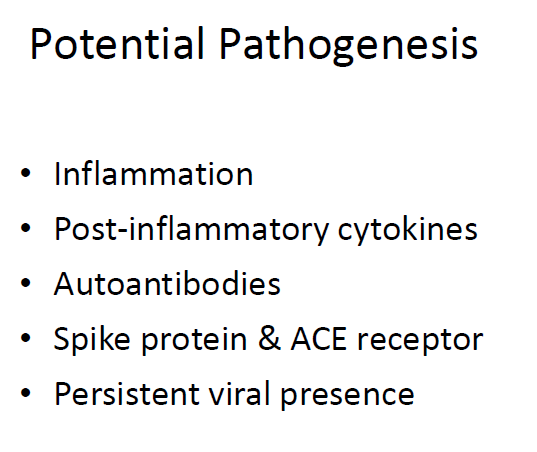
We are still trying to figure out the pathophysiology of #LongCOVID... these are just a few of the hypothesis. But definitely inflammation and immune system dysregulation is involved.
2/
2/
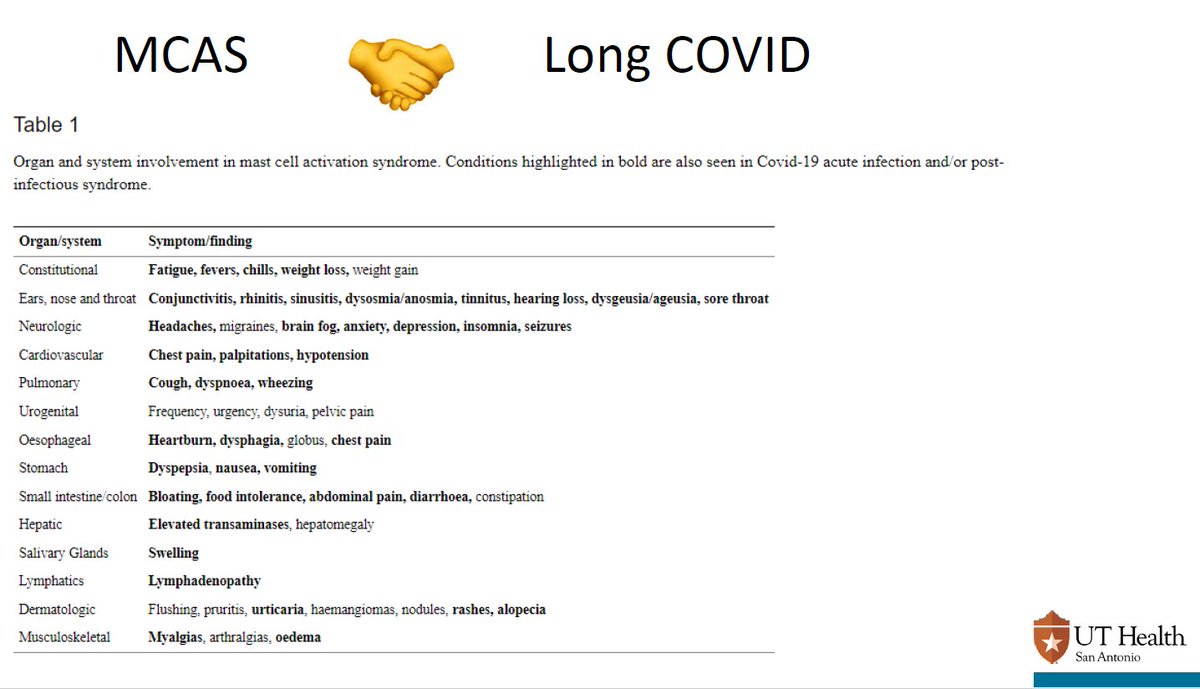
We also know #COVID19 hyperinflammation and #PASC may be rooted in mast cell activation syndrome #MCAS 3/
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…
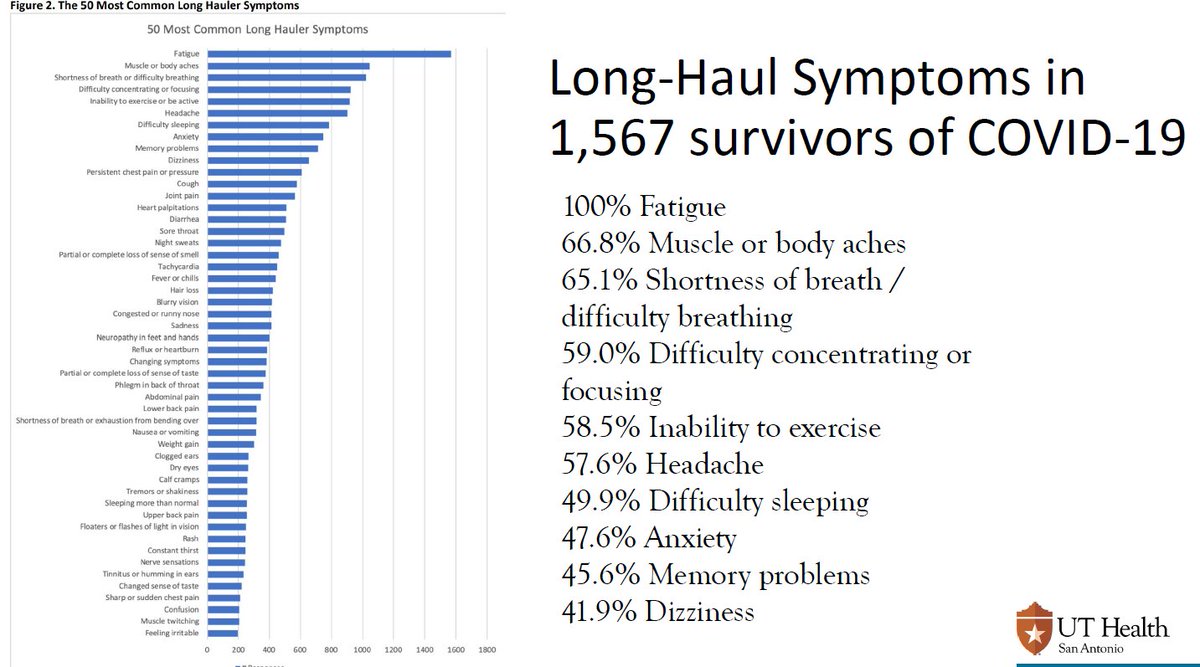
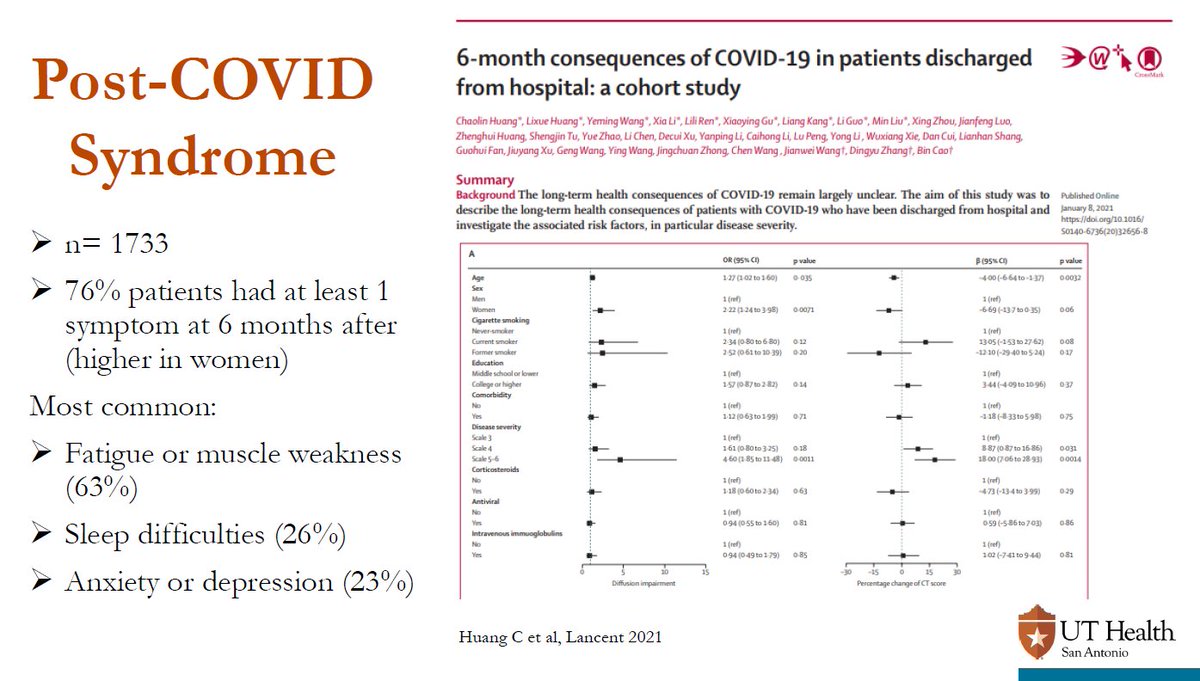
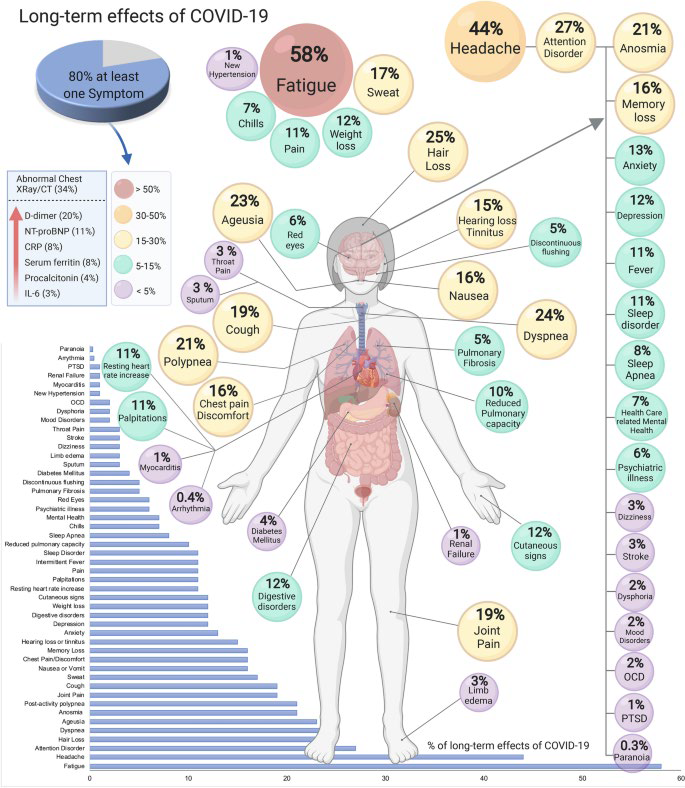
5/ What does recovery really look like?
(And I promise you most #LongCOVID patients did not have #CovidLungs - they had mild disease)
(And I promise you most #LongCOVID patients did not have #CovidLungs - they had mild disease)

8/ I have run a #LongCOVID clinic since August 2020 based on work I previously have done with TBI, stroke, dysautonomia, NeuroRehab, post-polio, critical illness recovery, and other post-viral illness like ME/CFS.
Getting close to 700+ persons seen.
Getting close to 700+ persons seen.
9/ I continuously learn from the patients & I know it's not enough time, research, or treatments. #TreatLongCovid 
10/ So much more to say on what we have been trying (but I need to go to clinic).
I was sure to emphasize topics often not taught in med school:
POTS
MCAS
ME/CFS
And to discuss health equity topics!
I was sure to emphasize topics often not taught in med school:
POTS
MCAS
ME/CFS
And to discuss health equity topics!
• • •
Missing some Tweet in this thread? You can try to
force a refresh