1/
In early residency, I was in a family meeting.
“Unfortunately, your 55yo loved one has suffered a very large stroke affecting a large portion of the brain. Surgery would reduce the change of death, but not the disability from the stroke.”
True or False? Vote below
In early residency, I was in a family meeting.
“Unfortunately, your 55yo loved one has suffered a very large stroke affecting a large portion of the brain. Surgery would reduce the change of death, but not the disability from the stroke.”
True or False? Vote below

2/
A #tweetorial, #EmoryNCCTweetorial, @medtweetorials about the role of decompressive hemicraniectomy in ischemic stroke.
Vote:
A #tweetorial, #EmoryNCCTweetorial, @medtweetorials about the role of decompressive hemicraniectomy in ischemic stroke.
Vote:
3/
First, I cringe now thinking about this statement, because I was the one that said it 😳😱.
This👏Is👏Not👏True👏
Fortunately, I was corrected. But, unfortunately, I have heard a version of this said on *numerous* occasions since then.
Why all the confusion?
First, I cringe now thinking about this statement, because I was the one that said it 😳😱.
This👏Is👏Not👏True👏
Fortunately, I was corrected. But, unfortunately, I have heard a version of this said on *numerous* occasions since then.
Why all the confusion?
4/
A tweetorial covering (goals for the scroll, if you will @sigman_md)
✅What is malignant edema & what's the natural history
✅The evidence for DHC in MCA stroke
✅ Why the hesitation and confusion about poppin' the top?
A tweetorial covering (goals for the scroll, if you will @sigman_md)
✅What is malignant edema & what's the natural history
✅The evidence for DHC in MCA stroke
✅ Why the hesitation and confusion about poppin' the top?
5/
“Malignant” MCA infarcts are complete, or near complete MCA territory infarctions which develop space-occupying mass effect which often results in herniation.
Much of what we know of the natural history was studied by Hacke et al (1996) pubmed.ncbi.nlm.nih.gov/8929152/
“Malignant” MCA infarcts are complete, or near complete MCA territory infarctions which develop space-occupying mass effect which often results in herniation.
Much of what we know of the natural history was studied by Hacke et al (1996) pubmed.ncbi.nlm.nih.gov/8929152/

6/
They prospectively eval'ed 55 pts w/ full territory MCA infarctions. Pt were 34-74 yo (avg 56). They were treated w/ intubation, hyperosmolar therapy, & barbiturates as needed (aggressive medical therapy).
💥78%💥 died despite maximal medical treatment with first 7 days.
They prospectively eval'ed 55 pts w/ full territory MCA infarctions. Pt were 34-74 yo (avg 56). They were treated w/ intubation, hyperosmolar therapy, & barbiturates as needed (aggressive medical therapy).
💥78%💥 died despite maximal medical treatment with first 7 days.
7/
Let’s contextualize this: ARDS sucks.
But our best estimates of death from ARDS is ~40% (pubmed.ncbi.nlm.nih.gov/26903337/). This is significant.
But, malignant middle cerebral ischemic edema?
~2x as deadly as ARDS 💀
Let’s contextualize this: ARDS sucks.
But our best estimates of death from ARDS is ~40% (pubmed.ncbi.nlm.nih.gov/26903337/). This is significant.
But, malignant middle cerebral ischemic edema?
~2x as deadly as ARDS 💀
8/
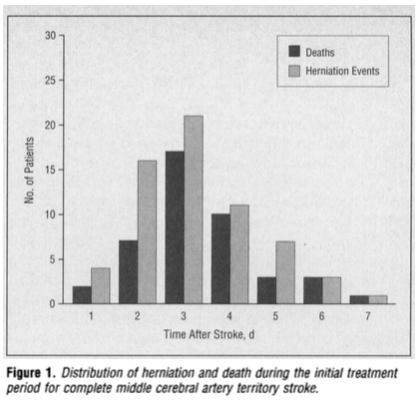
When exactly do these patients herniate & die?
The median day of herniation was day 4⃣. But just making it to day 4⃣ did not mean you were out of the woods. Half of the worsening happened after that point. This is important for later.
The pts who survived were the older pt
When exactly do these patients herniate & die?
The median day of herniation was day 4⃣. But just making it to day 4⃣ did not mean you were out of the woods. Half of the worsening happened after that point. This is important for later.
The pts who survived were the older pt
9/
So, we’re now all on the same page.
Full territory MCA stroke = bad. Particularly bad for young patients who have more robust edema responses and less atrophy to tolerate the swelling.
Medical therapy… *very* often fails.
Surgical therapy?
So, we’re now all on the same page.
Full territory MCA stroke = bad. Particularly bad for young patients who have more robust edema responses and less atrophy to tolerate the swelling.
Medical therapy… *very* often fails.
Surgical therapy?
10/
3 trials were published in the late 2000s to address this question: DESTINY I, DECIMAL, and HAMLET
All had some unique features.
Generally
👉Pts <60, w/ excellent functional baselines
👉All DHCs were completed b/f 96hrs;
👉Most were <48 hr (DESTINY<36hrs, DECIMAL<30hrs)
3 trials were published in the late 2000s to address this question: DESTINY I, DECIMAL, and HAMLET
All had some unique features.
Generally
👉Pts <60, w/ excellent functional baselines
👉All DHCs were completed b/f 96hrs;
👉Most were <48 hr (DESTINY<36hrs, DECIMAL<30hrs)
11/
Importantly, the patients did not have to have “full” territory infarctions. Most trials required ~2/3 of the territory with some basal ganglia involvement.
Big strokes, but not necessarily every. single. thing in the MCA territory.
Importantly, the patients did not have to have “full” territory infarctions. Most trials required ~2/3 of the territory with some basal ganglia involvement.
Big strokes, but not necessarily every. single. thing in the MCA territory.
12/
A pooled analysis of these trials was published in the Lancet in 2007 which looked at DHC which had been completed within *48 hours* of ictus of stroke.
pubmed.ncbi.nlm.nih.gov/17303527/.
The Result?
A pooled analysis of these trials was published in the Lancet in 2007 which looked at DHC which had been completed within *48 hours* of ictus of stroke.
pubmed.ncbi.nlm.nih.gov/17303527/.
The Result?

13/
Survival more than doubled, but contrary what seems to be a pervasive misunderstanding, the patients that survived were not often left totally dependent (mRS = 5). In fact, the rate of mRS 5 was very low.
43% of patients achieved an mRS of 2 or 3.
Survival more than doubled, but contrary what seems to be a pervasive misunderstanding, the patients that survived were not often left totally dependent (mRS = 5). In fact, the rate of mRS 5 was very low.
43% of patients achieved an mRS of 2 or 3.

14/
This of course is not a “perfect” outcome. Most of the patients enrolled had no prior disability.
So, yes, you can make case that surgery doesn’t “cure” the disability of stroke.
But is this a worthwhile outcome?
For many patients, absolutely.
A reminder about mRS:
This of course is not a “perfect” outcome. Most of the patients enrolled had no prior disability.
So, yes, you can make case that surgery doesn’t “cure” the disability of stroke.
But is this a worthwhile outcome?
For many patients, absolutely.
A reminder about mRS:

15/
Of course, is mRS even the right score to determine the worthiness of a pt’s life?
In DECIMAL 2/3 patients were living at home @ 1 yr
In HAMLET, pts & caregivers had low rates of being dissatisfied with tx.
Potentially biased? yes.
Demonstrative of human resiliency? yes.
Of course, is mRS even the right score to determine the worthiness of a pt’s life?
In DECIMAL 2/3 patients were living at home @ 1 yr
In HAMLET, pts & caregivers had low rates of being dissatisfied with tx.
Potentially biased? yes.
Demonstrative of human resiliency? yes.
16/
On the flip side, does decompressive hemicraniectomy guarantee a “good” outcome?
No.
Even with the most aggressive care, about 1 in 4.5 patients will go on to die of their stroke. That is not an insignificant number.
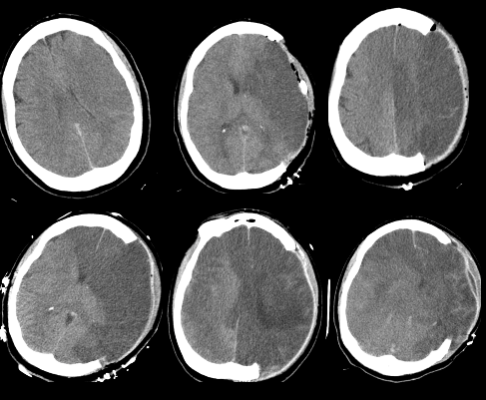
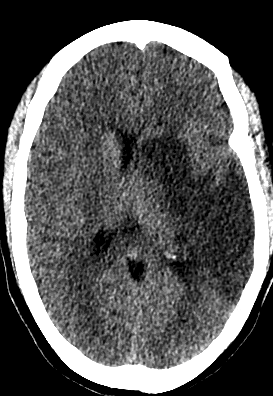
An example of progression despite surgery (Day 2-7)
On the flip side, does decompressive hemicraniectomy guarantee a “good” outcome?
No.
Even with the most aggressive care, about 1 in 4.5 patients will go on to die of their stroke. That is not an insignificant number.
An example of progression despite surgery (Day 2-7)
17/
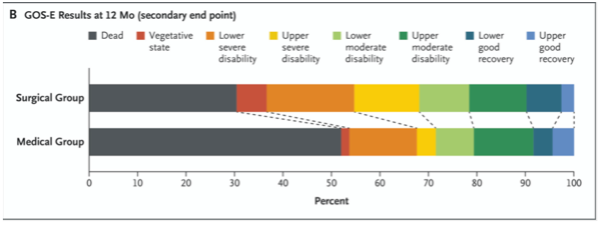
That said, the disability curve clearly shifts with DHC.
So why is there confusion?
I think there are 3 reasons:
1⃣ Surgery doesn’t reverse injury
2⃣ DHC has a different effect for older pts and in TBI
3⃣ Surgery is preventive not reactive
That said, the disability curve clearly shifts with DHC.
So why is there confusion?
I think there are 3 reasons:
1⃣ Surgery doesn’t reverse injury
2⃣ DHC has a different effect for older pts and in TBI
3⃣ Surgery is preventive not reactive
18/
Even the best surgery can’t take back the stroke.
Like many things in #NCC, our job is preventing 2⃣nd injury.
By reducing compression and herniation we prevent secondary injury ➡️ decreases disability + mortality.
This keeps being proven. Meta-analysis from 2021.
Even the best surgery can’t take back the stroke.
Like many things in #NCC, our job is preventing 2⃣nd injury.
By reducing compression and herniation we prevent secondary injury ➡️ decreases disability + mortality.
This keeps being proven. Meta-analysis from 2021.

19/
What is more likely to be muddling the picture is that all of the data above applies to *young patients* (<60 yo).
Things are more complicated >60yo. DESTINY II looked at DHC in the >60 group:
👉Only 6% attained an mRS=3.
👉19% of pt were left severely disabled. mRS 5.
What is more likely to be muddling the picture is that all of the data above applies to *young patients* (<60 yo).
Things are more complicated >60yo. DESTINY II looked at DHC in the >60 group:
👉Only 6% attained an mRS=3.
👉19% of pt were left severely disabled. mRS 5.

20/
Similarly, DHC for TBI is a different beast.
Charts from
DECRA (Left): poor outcomes on the left of bar
(⬆️in the DHC group).
And RESCUEicp (Right). Not a major change in the number of “good” outcomes w/ DHC; higher “bad” outcomes fill the mortality difference.

Similarly, DHC for TBI is a different beast.
Charts from
DECRA (Left): poor outcomes on the left of bar
(⬆️in the DHC group).
And RESCUEicp (Right). Not a major change in the number of “good” outcomes w/ DHC; higher “bad” outcomes fill the mortality difference.

21/
Finally, I don’t think this is the reason there is confusion, but I think there is sometimes hesitancy to take the bone off. Why?
B/c we this is often a preventive action. The patients may be doing ok at the time of the surgery.
Remember swelling peaks at day ~4
Finally, I don’t think this is the reason there is confusion, but I think there is sometimes hesitancy to take the bone off. Why?
B/c we this is often a preventive action. The patients may be doing ok at the time of the surgery.
Remember swelling peaks at day ~4
22/
The hope is to intervene b/f the midline shift, b/f the patient has transtentorial herniation that is making them sleepy (and aspirating)
But, I get it. This exposes a patient who seems to be “doing ok” to a surgical risk before they have demonstrated the need.
The hope is to intervene b/f the midline shift, b/f the patient has transtentorial herniation that is making them sleepy (and aspirating)
But, I get it. This exposes a patient who seems to be “doing ok” to a surgical risk before they have demonstrated the need.
23/
I like this example of a patient that was doing ok at hour 36 (CT scan on the left). Protecting airway, easily arousable. Kinda borderline size but had deep territory and the anterior temporal lobe infarcted.
By day 4 they would not have been doing well.

I like this example of a patient that was doing ok at hour 36 (CT scan on the left). Protecting airway, easily arousable. Kinda borderline size but had deep territory and the anterior temporal lobe infarcted.
By day 4 they would not have been doing well.

24/
So, the take-away here?
⭐️ DHC for malignant MCA edema improves BOTH a mortality & disability .
⭐️Data support early (w/I 48 hrs) action for young pts (<60yo) w/ large MCA stroke
⭐️Pls reach out & transfer these pts early if u don't have NSGY! 23% isn't going to fix this!
So, the take-away here?
⭐️ DHC for malignant MCA edema improves BOTH a mortality & disability .
⭐️Data support early (w/I 48 hrs) action for young pts (<60yo) w/ large MCA stroke
⭐️Pls reach out & transfer these pts early if u don't have NSGY! 23% isn't going to fix this!
25/
And finally, family/pts values matter so much here, this has to be a personalized convo! Thoughts? Additions? @aartisarwal @drdangayach @theABofPharmaC @emcrit @rkchoi @namorrismd @nsanar @ghoshal_shivani @PulmCrit @AaronLBerkowitz @karenccrx @EricLawson90 @Capt_Ammonia
And finally, family/pts values matter so much here, this has to be a personalized convo! Thoughts? Additions? @aartisarwal @drdangayach @theABofPharmaC @emcrit @rkchoi @namorrismd @nsanar @ghoshal_shivani @PulmCrit @AaronLBerkowitz @karenccrx @EricLawson90 @Capt_Ammonia
• • •
Missing some Tweet in this thread? You can try to
force a refresh