1/
We often check SPEP and/or immunofixation in patients with neuropathy. Why bother, and what should I do with the results?
Welcome to Paraproteinemic Neuropathy: A #tweetorial for neurologists who order tests they have no business interpreting.
We often check SPEP and/or immunofixation in patients with neuropathy. Why bother, and what should I do with the results?
Welcome to Paraproteinemic Neuropathy: A #tweetorial for neurologists who order tests they have no business interpreting.

2/
For starters, let's clear the air about terminology. These are all synonyms:
- Paraproteinemia
- Monoclonal gammopathy
- M-protein
- M component
They all mean identical plasma cells are overproducing identical copies of the same immunoglobulin or immunoglobulin fragments.
For starters, let's clear the air about terminology. These are all synonyms:
- Paraproteinemia
- Monoclonal gammopathy
- M-protein
- M component
They all mean identical plasma cells are overproducing identical copies of the same immunoglobulin or immunoglobulin fragments.

3/
Paraproteinemia is common as we age. It's usually benign (MGUS) and asymptomatic, but can be associated with almost ANY neuropathy syndrome.
(PSA: If you do a Google image search for Stocking and Glove looking for neuropathy pics, be prepared to find a bunch of S&M sites.)
Paraproteinemia is common as we age. It's usually benign (MGUS) and asymptomatic, but can be associated with almost ANY neuropathy syndrome.
(PSA: If you do a Google image search for Stocking and Glove looking for neuropathy pics, be prepared to find a bunch of S&M sites.)

4/
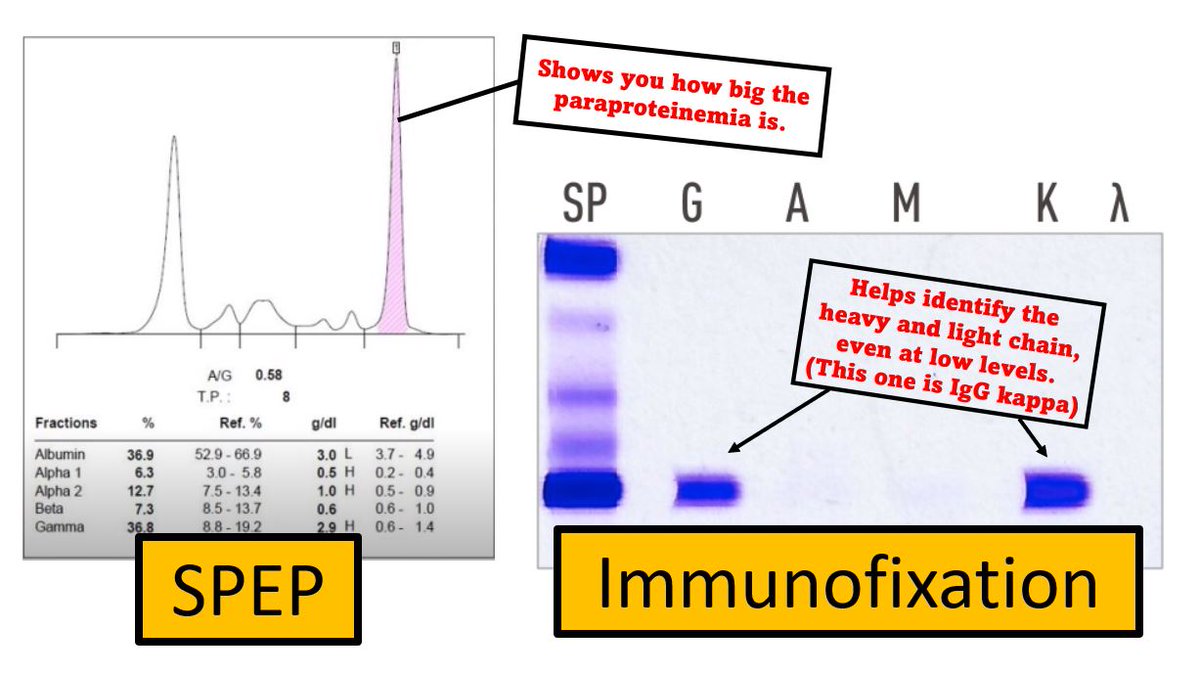
How do you test for it? Serum protein electrophoresis AND immunofixation. Getting both will help find low level gammopathies, which can still be associated with neuropathy!
UPEP, BJS, and free light chain ratio might help a little, but I don't include them as screening tests.
How do you test for it? Serum protein electrophoresis AND immunofixation. Getting both will help find low level gammopathies, which can still be associated with neuropathy!
UPEP, BJS, and free light chain ratio might help a little, but I don't include them as screening tests.
5/
Paraproteins will be reported with three pieces of information:
A heavy chain (IgG, IgA, or IgM)
A light chain (kappa or lambda)
A concentration (i.e. 0.6 g/dL)
Almost any other info they report (polyclonal gammopathy, etc.) is probably not useful to neurologists. Fight me.
Paraproteins will be reported with three pieces of information:
A heavy chain (IgG, IgA, or IgM)
A light chain (kappa or lambda)
A concentration (i.e. 0.6 g/dL)
Almost any other info they report (polyclonal gammopathy, etc.) is probably not useful to neurologists. Fight me.

6/
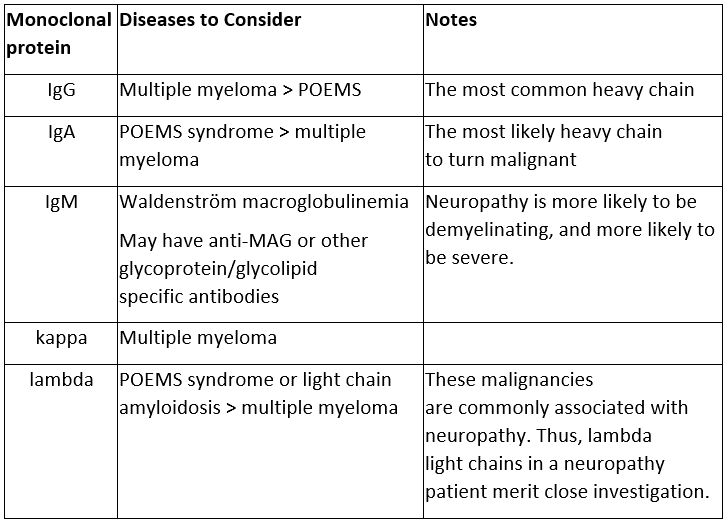
Different heavy and light chains are associated with different malignancies. Get to know which with this handy chart.
As for me, my heart beats a little faster when I find an IgM heavy chain or a lambda light chain paraproteinemia.
Different heavy and light chains are associated with different malignancies. Get to know which with this handy chart.
As for me, my heart beats a little faster when I find an IgM heavy chain or a lambda light chain paraproteinemia.
7/
The concentration (or level) correlates with the risk of malignancy.
Low levels, like 0.1 g/dL, are almost always MGUS.
High levels, like 3.0 g/dL = DANGER.
(Is it any wonder that the immunoglobulin fragments can so easily be rearranged to make the #Decepticon symbol?)
The concentration (or level) correlates with the risk of malignancy.
Low levels, like 0.1 g/dL, are almost always MGUS.
High levels, like 3.0 g/dL = DANGER.
(Is it any wonder that the immunoglobulin fragments can so easily be rearranged to make the #Decepticon symbol?)

8/
Neuropathy may be the first symptom of a heme malignancy, so neurologists may be the first to realize something serious is going on.
Are we heroes? Well, I wouldn't necessarily use that term. People do call us that, though.
So when should we worry and refer to heme-onc?
Neuropathy may be the first symptom of a heme malignancy, so neurologists may be the first to realize something serious is going on.
Are we heroes? Well, I wouldn't necessarily use that term. People do call us that, though.
So when should we worry and refer to heme-onc?

9/
Consult heme-onc for:
1. IgA heavy chain (IgA probably has the highest risk of malignant transformation.)
2. Paraprotein level >1.5 g/dL. (If lower, just check annually.)
3. Anemia, renal failure, hypercalcemia.
4. Lytic or sclerotic lesions on bone scan or skeletal survey
Consult heme-onc for:
1. IgA heavy chain (IgA probably has the highest risk of malignant transformation.)
2. Paraprotein level >1.5 g/dL. (If lower, just check annually.)
3. Anemia, renal failure, hypercalcemia.
4. Lytic or sclerotic lesions on bone scan or skeletal survey

10/
Take home:
- Neuropathy ▶️check SPEP and IFIX
- Paraproteinemia▶️check CBC, Cr, Ca, bone scan and refer to heme-onc for abnormalities
- For bonus life points, learn which heavy and light chains are associated with different neuropathy syndromes and malignancies!
Take home:
- Neuropathy ▶️check SPEP and IFIX
- Paraproteinemia▶️check CBC, Cr, Ca, bone scan and refer to heme-onc for abnormalities
- For bonus life points, learn which heavy and light chains are associated with different neuropathy syndromes and malignancies!

11/
For a little more information, but a little less fun, see my @AANMember Neurobyte on this topic. learning.aan.com/diweb/catalog/… #MedEd #neurotwitter #neurotwitternetwork #futureneurologist @AANEMorg
For a little more information, but a little less fun, see my @AANMember Neurobyte on this topic. learning.aan.com/diweb/catalog/… #MedEd #neurotwitter #neurotwitternetwork #futureneurologist @AANEMorg
• • •
Missing some Tweet in this thread? You can try to
force a refresh